Managing medical billing in-house can be complex, costly and take up a huge amount of your staff’s time. These are just some of the reasons the demand for medical billing outsourcing services is rapidly growing. According to Market Research Future, the medical billing market size is expected to grow from $17.76 billion in 2024 to $32.79 billion by 2032, at a compound annual growth rate (CAGR) of 12.14%. If you’ve decided to outsource your revenue cycle management (RCM), choosing the right medical billing company is the key to sustained success. Each stage in the claim submission process needs to be completed efficiently and accurately to ensure that you receive appropriate reimbursement for services rendered. That’s why it’s important to have the right support. Ultimately, with an expert handling the financial and administrative aspects of your practice, you would have more time for what really matters – patient care.


Ready to take control of your medical billing and enhance your practice’s financial management?
Factors to Consider when Choosing a Medical Billing Company
Here’s our top criteria to consider when choosing a billing service for your medical practice. 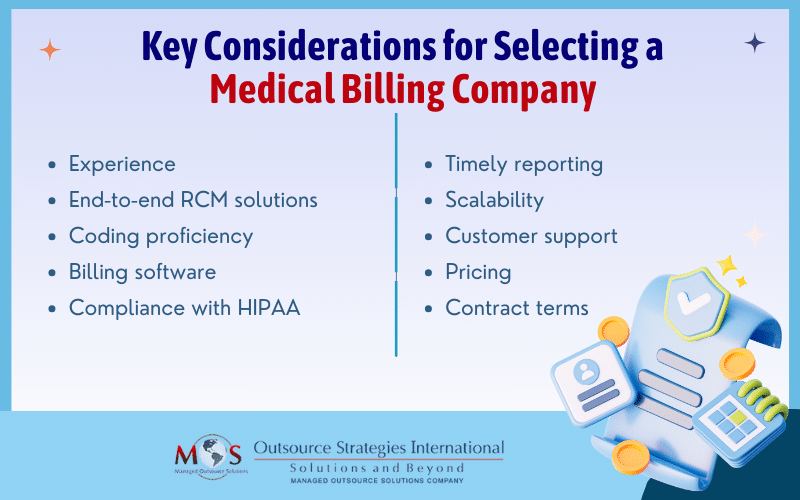
- Experience: With complex rules, regulations and codes, billing for healthcare services is difficult. When you choose an experienced company, you can rest assured that you have an expert handling the process. They will have in-depth knowledge of all aspects related to billing for medical services and stay up to date with rules, compliance requirements, and best practices. They’ll have experience with almost all billing scenarios and know how to handle them. With their experience in dealing with different payers, they’ll be able to resolve payer-specific problems. Additionally, always make sure to partner with a company that has experience in your specialty.
- End-to-end RCM solutions: Choose a company that provides the entire gamut of RCM services. Comprehensive and customized RCM solutions include everything from patient registration, insurance eligibility verification, and medical coding to charge entry, cash posting and reconciliation, claim generation and submission, to accounts receivable and denial management. An ideal partner will have a team of billing specialists that can handle each step of the full RCM process.
- Coding proficiency: Coding errors are one of the most common reasons for denials. Choosing a company that has AAPC-certified professionals with expertise in ICD-10 and CPT coding is crucial. Experienced coders can read and interpret medical records with the required attention to detail and assign the correct codes. They can also contact providers when needed to ensure correct code assignment and proper payment.
- Billing software: The company you choose should use billing software and technology that is compatible with your practice management system. Finding a partner that is proficient in using the latest technology that can automate the billing process can be extremely helpful in eliminating manual errors.
- Compliance with HIPAA and other regulations: Adhering to stringent industry regulations such as HIPAA and Anti-Kickback Laws is a fundamental requirement in billing. Choose a company that guarantees HIPAA compliance when handling of your practice’s protected health information (PHI). A reliable billing company can ensure that PHI is appropriately and securely maintained and shared only as required. They’ll also focus on maintaining billing accuracy to uphold the standards outlined in Anti-Kickback Laws.
- Timely reporting: Make sure the company you choose provides regular reports. Consistent reporting is imperative for tracking the financial performance of your practice, identifying any roadblocks and allowing you to address them promptly. Clear and transparent reports can provide insights into the complete revenue cycle, enabling your practice to assess key metrics, recognize trends, and make data-driven decisions.
- Scalability: The billing company you choose should be able to customize their services to your practice’s specific needs. They should be able to deliver scalable solutions while making sure service quality and efficiency are not compromised.
- Customer support: Excellent customer support is essential in medical billing. Ask about availability and average response times, especially when billing errors or issues occur. Ideally, the company you choose will have a dedicated customer support team to quickly address questions or concerns.
- Pricing: It may seem obvious but be sure to ask about the company’s pricing structure and any possible fees. Be aware of their payment model – some billing companies charge a percentage of collections or a flat fee, and some a combination of both. Ideally, you will want to find a company and pricing structure that can help you save 30-40% on your operational costs. Some initial quotes do not include any hidden fees or charges, so always ask if any are included.
- Contract terms: Always carefully review the full contract terms and conditions before signing up. Evaluate factors such as contract length, termination clauses, confidentiality agreements, and any other provisions that may affect your working relationship to be sure everything meets your practice’s needs.
Carefully evaluating all these criteria will help you choose a billing service that best suits your practice. A couple more quick tips – don’t forget to check out client testimonials, and it’s always best to start with a free trial if possible. Many of the top medical billing companies offer a free trial, allowing you to assess their performance risk free and make an informed decision about a potential partnership.


Modernize your billing process. Experience expert guidance and optimized revenue cycles.
Call (800) 670-2809!




