Every year, claim denials result in substantial losses for healthcare providers. Managing denied claims is a crucial element in healthcare revenue cycle management (RCM). Denial management services focus on identifying, analyzing, and addressing the underlying causes of claim denials. These services focus on pinpointing patterns, assessing coding and documentation errors, and implementing corrective measures to reduce future denials. Today, AI is changing the game in denial management.
According to a report from the American Academy of Family Physicians (AAFP), the average claim denial rate across the healthcare industry is between 5% to 10%. Medical claim denials occur when a payer denies reimbursement due to coding errors, non-covered services, or lack of medical necessity.
Struggling with claim denials?
Minimize rejections and enhance cash flow with our denial management services!
Traditional denial management methods rely on manual processes to identify, analyze, and resolve claim denials. These approaches are time consuming and tedious, often involve reviewing denied claims individually, tracking denial trends using spreadsheets, and manually appealing rejected claims.
This post discusses common denial management challenges and how AI is transforming the process by enhancing efficiency, accuracy, and predictive capabilities.
Common Claim Denial Management Challenges
Denial management comes with several challenges that can impact revenue cycle efficiency and financial stability. Some common issues include:
- Lack of real-time visibility: Healthcare organizations struggle with Keeping track of denials due to disorganized data and outdated reporting systems.
- Complex and changing payer policies: Frequent changes in insurance policies, coding regulations, and medical necessity requirements make it difficult to stay compliant and prevent denials.
- Lack of standardization: The lack of standardization is another issue. Each payer has its own rules for rejecting claims and notifying providers. As a result, there is no uniform strategy for healthcare providers and payers to analyze denial data effectively.
- Coding and documentation errors: Medical coding mistakes, incomplete documentation, and missing prior authorizations are leading causes of claim denials.
- Incorrect or missing patient information: Claims are denied if there are errors in name spellings, date of birth mismatches, invalid insurance details, incomplete demographic data and technical errors. This is usually the result of lack of proper patient eligibility verification.
- High administrative burden: Managing denials requires significant staff time and effort, increasing operational costs and diverting resources from other critical revenue cycle tasks.
- Recurring denial trends: Without proper root cause analysis, organizations may repeatedly face similar denial issues, leading to ongoing revenue losses.
- Slow and inefficient manual processes: Many providers still rely on manual workflows, making it difficult to proactively detect and prevent denials. Manually reviewing and appealing denied claims is time-consuming, requiring extensive communication with payers and resubmission efforts.
By integrating AI and automation, healthcare organizations can significantly reduce denial rates, optimize RCM, and boost overall operational efficiency.
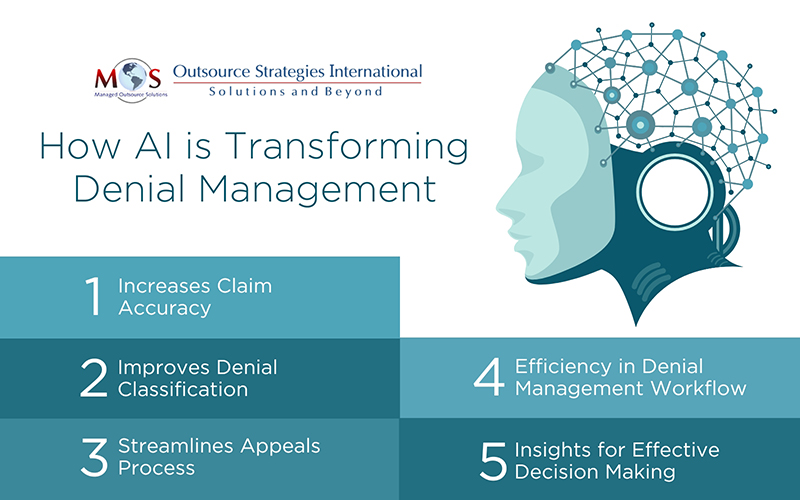
How AI is Changing Denial Management
- Increases Claim Accuracy
Machine learning algorithms help predict potential denials before submission, reducing errors related to coding, documentation, medical necessity, and ensuring compliance with payer rules.
- AI automates patient data collection, ensuring accurate billing codes, service details, and required claim information.
- Natural language processing (NLP) extracts relevant details from medical records to improve documentation accuracy.
- AI-driven tools also streamline claim scrubbing, reducing manual effort and increasing first-time claim approval rates.
- Machine learning analyzes past claims to identify patterns in denials, helping prevent errors before submission.
- Improves Denial Classification
AI streamlines denial identification and categorization by automatically analyzing claim data, detecting patterns, and classifying denials based on root causes. Machine learning and natural language processing (NLP) quickly sort denials by payer rules, coding errors, or documentation issues, enabling faster resolution and improved revenue cycle efficiency.
By categorizing and prioritizing denials, automation allows denial management teams to quickly spot systemic issues and address urgent claims, preventing cash flow delays.
- Streamlines Appeals Process
By analyzing past denials and payer trends, AI helps prioritize claims with higher chances of approval, reducing manual effort and processing time. AI-powered automation transforms the appeal process by:
- Identifying denial reasons
- Retrieving relevant documentation
- Generating accurate appeal letters
Automated workflows ensure appeals are submitted promptly, minimizing delays and increasing the likelihood of successful reimbursement. This results in faster resolutions, improved cash flow, and reduced administrative burden.
- Efficiency in Denial Management Workflow
AI enhances the denial management workflow by automating key processes, reducing manual workload, and improving accuracy.
- Frees up staff for critical tasks and increases productivity
- Integrates with the RCM system, improving visibility into the RCM process, from claim submission to final resolution, supporting denial management.
- Enhances coordination among billing, coding and denial management teams, supporting faster claim resolution.
- Insights for Effective Decision Making
AI-driven data insights play a crucial role in optimizing denial management by identifying trends, root causes, and high-risk claims.
- Analyzes large volumes of claims data to detect recurring denial patterns
- Predicts potential rejections and provides real-time alerts
- Allows for implementing proactive strategies before issues escalate
Advanced analytics offer real-time visibility into denial rates, payer behavior, and coding errors, enabling data-driven decision-making. These insights help refine billing and documentation practices, enhancing claim approval rates.
AI in Denial Management: Balancing Technology with Human Expertise
Leveraging AI and automated processes can help ensure your practice has lower denial rates and a healthy cash flow. AI will continue to transform denial management strategies by improving predictive analytics, automating workflows, and improving claim accuracy. Future advancements in machine learning and NLP will further refine denial prevention strategies, making RCM more efficient and proactive.
However, despite these technological breakthroughs, the human element remains irreplaceable when it comes to managing denials in medical billing. Skilled professionals are essential for interpreting complex cases, handling nuanced payer negotiations, and ensuring ethical decision-making. The most effective denial management approach will combine AI-driven automation and human expertise, enabling healthcare organizations to maximize efficiency while maintaining accuracy, compliance, and quality patient care.
Don’t let denials disrupt your cash flow!
Partner with us for superior denial management solutions and maximize revenue!




