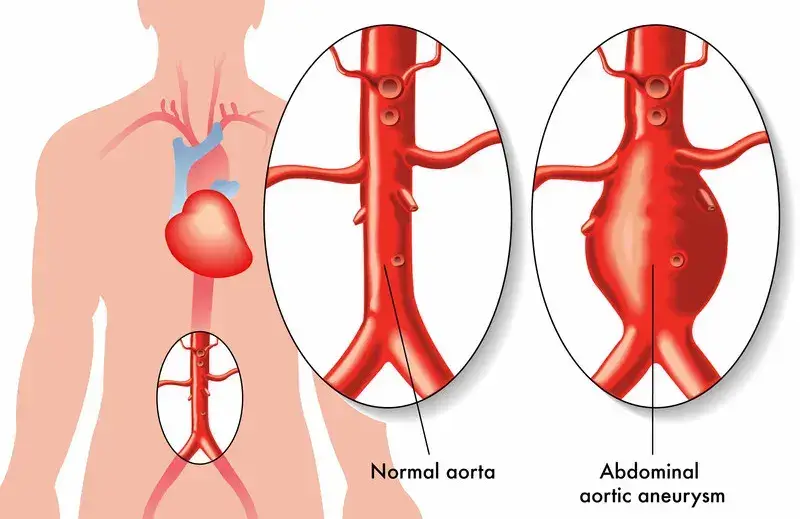
Abdominal aortic aneurysm (AAA) is a bulge or swelling in the lower part of the aorta – one of the largest blood vessels in the human body. The aorta circulates blood from the heart and lungs to the rest of the body including the chest, abdomen, pelvis and lower limbs. The condition occurs when an artery expands (like a small balloon) to more than one and a half times its normal size, if it becomes weak. An AAA can be risky, if it is not detected early and treated appropriately. Aortic aneurysms can get bigger in size over time and could rupture, (burst) causing life-threatening complications like bleeding. For proper clinical documentation of this disorder, physicians can rely on medical billing outsourcing services.
Reports suggest that about 200,000 people in the United States are diagnosed with abdominal aortic aneurysm (AAA) every year. It is estimated that ruptured AAAs account for roughly 4% to 5% of sudden deaths in the US. Abdominal aortic aneurysm is generally classified as small and large based on their size and the speed at which they are growing. The size and speed of growth are the two main factors that help decide the treatment options, which in most cases may range from careful observation/monitoring to emergency surgery.
Who Is at Risk for an AAA?
Abdominal aortic aneurysm is more likely to occur if you are –
- Male above the age of 60 years
- Obese/overweight people
- Have a family history of heart diseases/conditions
- Have a high blood pressure
- Have high cholesterol or fatty buildup in the blood vessels (atherosclerosis)
- Lead a sedentary lifestyle
- Have a habit of smoking
- Previous aneurysms in other arteries in the legs or chest
- Have had trauma to your abdomen or other damage to your midsection
- Bacterial of fungal infection in the aorta
Identifying the Symptoms
Generally, AAA is quite difficult to detect as they grow slowly without any visible symptoms. In some cases, certain types of aneurysms will never rupture. If an AAA does rupture, people experience one or more of the following symptoms –
- Sudden pain in your abdomen or back
- Shock or loss of consciousness
- Pain spreading from your abdomen or back to your pelvis, legs, or buttocks
- Increased heart rate
- Clammy or sweaty skin
- A pulsating feeling near the navel
- Dizziness
- Shortness of breath
- Vomiting
- Low blood pressure
If any of the above signs and symptoms like sudden severe back or abdominal pain is experienced, it is important to seek emergency medical help.
Screening Guidelines and Diagnosis
USPSTF Screening Guidelines
The following guidelines are issued by U.S. Preventive Services Task Force (USPSTF)for screening abdominal aortic aneurysm (AAA) –
- Men aged 65 to 75 years who have ever smoked should have a one-time for abdominal aortic aneurysm (AAA) with ultrasonography. Men aged 60 years and older with a family history of abdominal aortic aneurysms should consider regular screening for the condition.
- Clinicians selectively offer screening for AAA in men aged 65 to 75 years, who have never smoked rather than routinely screening all men in this group.
- The USPSTF recommends against routine screening for AAA in women who have never smoked.
Diagnosing and Coding AAA
Abdominal aortic aneurysms (AAAs) are often diagnosed during a detailed clinical examination. For instance, during a routine clinical examination, if your physician feels/suspects a pulsating bulge in your abdomen, they may request specialized diagnostic imaging tests such as – chest X-ray, abdominal ultrasound, CT scan of the abdomen and abdominal MRI to confirm the same. Treatment for this condition includes – careful medical monitoring or surgery, which aims to prevent the aneurysm from rupturing. Depending on the size, rate of growth and exact location of the aneurysm, physicians may perform surgery to repair or remove the damaged tissue.
For a small AAA, physicians may choose careful medical monitoring instead of performing surgery. If the physician notices that your aneurysm is small (less than 5.5 centimeters wide) and not experiencing any specific symptoms, he/she may recommend medical monitoring (which involves regular monitoring of the growth of the aneurysm and management of other medical conditions that could potentially worsen your symptoms). Physicians will also recommend regular imaging tests to check the size of aneurysm. The frequency of imaging tests depends on the size of the aneurysm, whether the aneurysm is growing and how fast it’s growing.
Surgical procedures include open abdominal surgery and endovascular surgery (based on severity of symptoms and size of growth). Open abdominal surgery, a more invasive form is performed if your aneurysm is very large or has already ruptured. Endovascular surgery – a less invasive form of surgery on the other hand, uses a graft to stabilize the weakened walls of your aorta. Recovery from open abdominal surgery may take up to 6 weeks, where as endovascular surgery may only take about 2 weeks to recover fully.
Medical Codes to Use
Vascular medical coding involves the use of specific ICD-10 codes to document any such conditions, including abdominal aortic aneurysms (AAA). ICD-10-CM codes used to indicate a diagnosis of AAA for reimbursement purposes include –
- I71 – Aortic aneurysm and dissection
- I71.0 – Dissection of aorta
- I71.00 – Dissection of unspecified site of aorta
- I71.3 – Abdominal aortic aneurysm, ruptured
- I71.4 – Abdominal aortic aneurysm, without rupture
- I71.8 – Aortic aneurysm of unspecified site, ruptured
- I71.9 – Aortic aneurysm of unspecified site, without rupture
The success of surgical treatment procedures and recovery may predominantly depend on the fact whether or not the AAA was found before it ruptures. Diagnosing the condition early (before it ruptures) will help in better treatment. For people diagnosed with AAA, physicians may recommend avoiding rigorous physical activity and heavy lifting that can put additional pressure on your aneurysm and increase the blood pressure level. Focusing on heart health by taking certain steps such as keeping blood pressure and cholesterol under control, avoiding tobacco products, regular exercise and eating a healthy diet can prevent the condition in the long run.
Medical coding for different vascular conditions can be complicated. For accurate and timely medical billing and claims submission, healthcare practices can outsource their medical coding tasks to a professional medical billing company that provides the services of AAPC-certified coding specialists.