For any healthcare practice, accurate billing of medical claims is crucial to enhance financial stability and operational efficiency, optimize revenue cycles and maintain a steady cash flow. Precise billing helps minimize errors and claim denials, ensuring a smooth reimbursement process.
So why should you outsource healthcare billing tasks? Utilizing medical billing services is a strategic move that healthcare practices can make to submit clean, error-free medical claims to insurers. In the dynamic landscape of healthcare, where precision and efficiency are paramount, the decision to outsource is proving to be a game-changer for practitioners. Outsourced medical billing benefits include streamlined processes, reduced errors, and enhanced financial efficiency, allowing healthcare practices to focus on delivering optimal patient care.

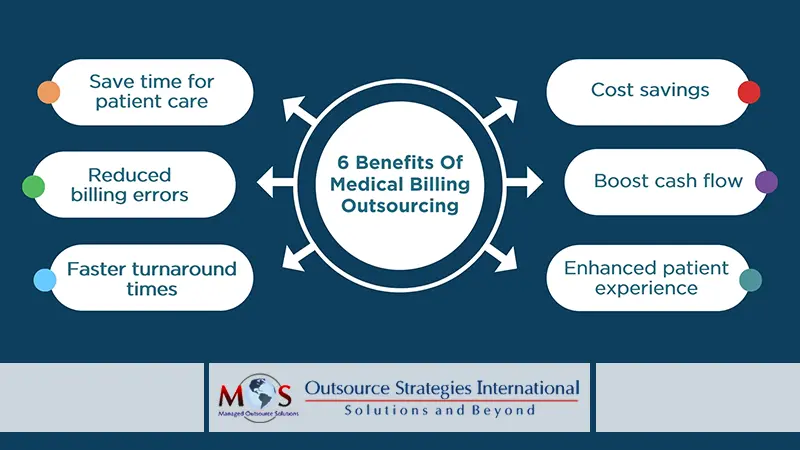
Benefits of Medical Billing Outsourcing
Why Outsource Medical Billing?
Here’s a closer look at the major benefits that come with entrusting your billing processes to seasoned professionals:
- Focus on core competencies: With these services provided by experienced hands, providers can devote more time to patient care. This is specifically advantageous for smaller physician groups that cannot afford a large office staff. The efficiency of physicians in delivering exceptional patient care is hindered when they are burdened by the financial responsibilities associated with managing a practice.
- Cost savings: Managing an in-house team leads to significant overhead costs, including salaries, benefits, and ongoing training. Outsourcing the task enables providers to optimize resource utilization and enhance overall efficiency in revenue cycle management. Practices can access specialized services without the financial burden of maintaining an entire billing department.
- Reduced documentation errors: Professional billing companies are well-versed in the intricacies of coding and compliance. This expertise minimizes the risk of errors and claim denials, ensuring accurate and timely reimbursement for services rendered. Expert medical billers are knowledgeable about the complex healthcare billing and coding standards and healthcare terminology related to the specialty they deal with. Medical claims with fewer errors ensure a healthy revenue cycle.
- Enhanced cash flow: Outsourcing accelerates revenue collection, providing a steady financial foundation for sustained growth and operational excellence. The reduction in overhead costs, timely submission of claims and increased reimbursements will also result in increased revenue for the firm.
- Enhanced patient experience: Improved accuracy in billing statements and reduced discrepancies contribute to greater patient satisfaction. By entrusting billing processes to dedicated professionals, healthcare providers can streamline administrative tasks, reduce documentation errors, and expedite claims processing. This efficiency translates to quicker reimbursement cycles, minimizing delays in providing patients with accurate and transparent financial information. The positive impact on billing transparency, reduced wait times, and increased focus on patient interactions collectively contribute to an enhanced overall experience for patients.
- Quick turnaround time: By entrusting these responsibilities to dedicated medical billing teams, healthcare providers can expedite the entire revenue cycle-from claim submissions to reimbursement. Outsourcing ensures that such tasks are handled promptly and accurately, reducing the time it takes to process claims and receive payments.
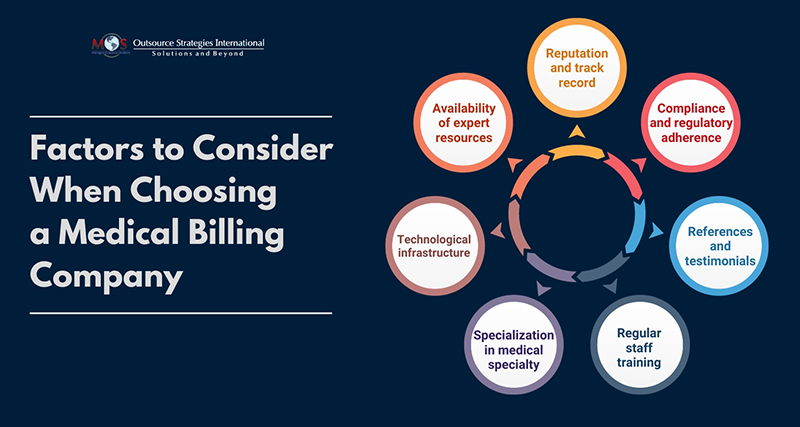
What Actually Matters – Choosing the Right Partner to Outsource
Selecting the right healthcare billing company is a critical decision that profoundly influences the financial health and operational efficiency of a healthcare practice. It necessitates a meticulous evaluation of several key factors. A professional service provider should have a proven track record of accuracy, timely reimbursements, and compliance with industry regulations. Transparency in communication, including detailed reporting and regular updates, is paramount for a successful partnership.
The company’s technological infrastructure and adaptability to evolving healthcare standards is critical to a seamless integration with the practice’s existing systems. Additionally, understanding the company’s expertise in the specific specialty or field is crucial. Ultimately, a comprehensive assessment of the company’s reputation, expertise, technology, and communication practices ensures that healthcare providers make an informed choice, laying the foundation for a successful and collaborative partnership.


Revolutionize your practice’s financial management with our medical billing outsourcing services.