The diagnosis and treatment for spinal care can be complex, and requires a multidisciplinary team of healthcare specialists – neurosurgeon, orthopedic surgeon, physical therapist, chiropractor and others – to provide integrated patient care. To ensure timely payments for these providers, a billing and coding team dedicated to spinal care should ensure proper claims submission with accurate medical codes. Physicians use precise medical terminology to communicate their observations and prescriptions, and coders and billing staff should be knowledgeable about these terms to be able to report the various diagnoses and medical services to third-party payers.
Spine-related pain may be associated with nerve root compression, facet arthropathy, and other conditions. Diagnostic spinal procedures offered may include lumbar puncture, myelography, discography, biopsy and aspiration along with plain film radiography, nuclear medicine, CT, and MRI studies. Coding spine surgeries is challenging, but professional coders can assign the appropriate codes to describe the services as they have a proper understanding of the spinal anatomy and terminology.
The billing process includes the following:
- The surgeon ranking the most complex surgery performed as the primary surgery
- Accurately coding for decompression/ discectomy with appropriate standalone and associated add-on codes
- Billing for fusion/ arthrodesis
- Billing for instrumentation/medical device
- Billing for any additional procedure performed
Pain management billing outsourcing is an ideal option for providers to simplify their billing process. An established pain management medical billing company will submit medical bills and claims within the specified time limit and maximize cash flow.
Need help to optimize reimbursement for your pain management services?
Talk to our experts!
Best Practices for Accurate Spine Billing and Coding
As coding errors can lead to charge capture errors and missed opportunities for payment, it is critical for medical coders to follow certain strategies to improve spine and pain management documentation and charge capture.
Here are some tips for successful spine and pain management medical billing and coding. These will help you navigate the intricate process of coding, comply with the legal framework changes and secure optimal revenue.
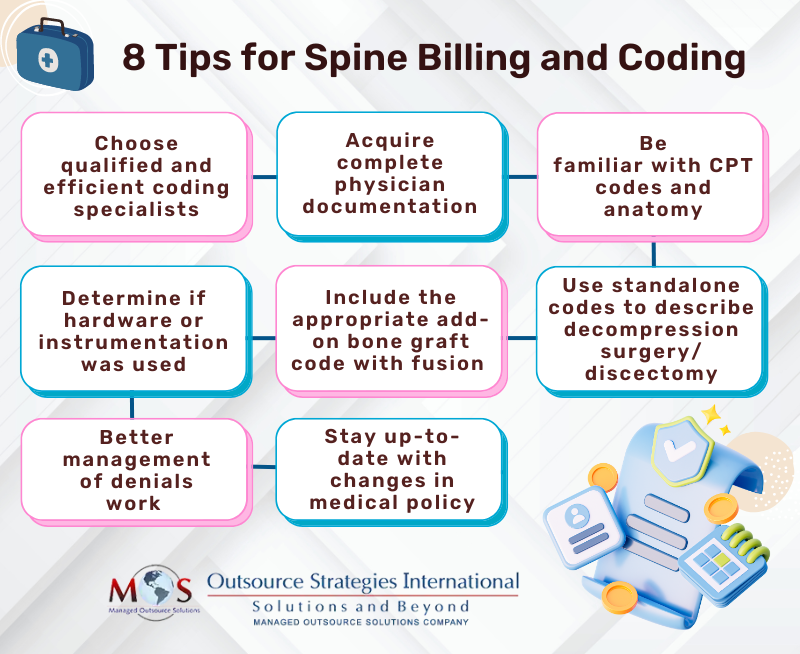
- Choose efficient medical coding specialists
The coders must be able to match the spinal nerves involved in a particular surgery to the proper code and assign an accurate number of levels. The coding staff should also thoroughly research appropriate coding practices for each new medical device to ensure claim approval.
- Acquire complete and detailed physician documentation
Physicians must provide complete and detailed operative notes and implant logs to make sure that medical coders assign the right medical codes. Inaccurate or incomplete documentation is a major reason for claim denials. Lack of relevant details may confuse the coder especially if multiple procedures were performed on a patient, resulting in coding errors.
So, physicians, in their operative notes, must clearly include the aim of the procedure and how it is performed along with matching modifiers. For instance, in spine surgeries, decompression documentation should specify each nerve targeted at each level. Before coding a new surgical approach, coders must understand whether new techniques are considered open or endoscopic procedures.
To assign the correct codes for spinal procedures, coders will examine the documentation to ensure that the following details are available:
- Location: cervical, thoracic, lumbar or sacral (the 33 vertebrae are classified as 7 cervical: C1-C7; 12 thoracic: T1-T12; 5 lumbar: L1-L5; 5 Sacral, and 4 Coccygeal vertebrae
- Approach: anterior, posterior or lateral extracavity, or percutaneous
- Pathology: what was done and medical indication (decompression, disc-ectomy, corpectomy, arthrodesis)
- Bone grafting: allograft or autograft
- Instrumentation: rods, screws or cages
- Implants used
- Get familiar with CPT codes and anatomy
Medical coders should be knowledgeable about the full anatomy of the spine, which helps them to interpret the correct operative note for surgical approach, level assignment and diagnosis assignment. Error-free CPT and ICD coding would depend on identifying which portion of the spine the physician is working on to determine the approach used and level assignment for a particular procedure.
For example, take spinal fusion (arthrodesis). The location reflects the level of the vertebrae (cervical, thoracic, lumbar and/or sacral) and the number of vertebral joints fused. ICD-10 codes can reflect the complexity of the procedures performed. However, correct ICD coding depends on having the following details:
- The information required to accurately assign the characters of a spinal fusion procedure code.
- The procedures that are considered integral to the fusion and assigned separate codes, and those are not integral to the fusion and not assigned additional codes.
- The number of fusion codes to assign (this depends on how many levels were fused).
As fusion is the merging of adjacent parts, the standalone CPT code for the fusion (synonymous with “arthrodesis,” or the joining of two or more vertebrae) should be assigned. For a single fusion segment that involves adjacent vertebral segments L4 and L5, the appropriate CPT code is:
- 22612 Arthrodesis, posterior or posterolateral technique, single level; lumbar (with lateral transverse technique, when performed)
If multiple vertebral joints are fused, a separate procedure is coded for each vertebral joint that used a different device and/or qualifier. For e.g.
- Fusion of lumbar vertebral joint, posterior approach, anterior column
- Fusion of lumbar vertebral joint, posterior approach, posterior column
To assign the appropriate CPT and ICD-10 codes, the pain management medical coding company should obtain proper and accurate information from the surgeon.
- Use standalone codes to describe decompression surgery/discectomy
Spinal decompression surgery can be performed anywhere along the spine from the neck. It involves the removal of the spinal disc, bone, or tissue causing pressure and pain. If this is the only procedure performed, then choose the appropriate standalone codes as they don’t have any additional add-on codes.
Check out some examples of standalone codes for decompression and discectomy:
- Laminectomy to decompress spinal canal and/or nerve roots: CPT codes 63001-63017, 63045 – +63048
- Discectomy to decompress spinal canal and/or nerve roots: 63020 – +63035, 63040 – +63044, 63055 – +63057
- Corpectomy: 63081 – +63091 (To use these codes, the documentation should also reflect removal of at least 50 percent of the cervical vertebral body, or 33 percent of the thoracic and lumbar vertebral bodies)
- Fracture repair: 22325 – +22328
The coder should examine the operative report to:
- Identify the presenting diagnosis
- Identify which decompression/discectomy activity was performed
- Identify whether the approach was posterior or anterior
- Assign the appropriate standalone code and any associated add-on codes
New Tethering Codes for 2024
- 22836 (Anterior thoracic vertebral body tethering, including thoracoscopy, when performed; up to 7 vertebral segments)
- 22837 (Anterior thoracic vertebral body tethering, including thoracoscopy, when performed; 8 or more vertebral segments)
- 22838 (Revision (e.g. augmentation, division of tether), replacement, or removal of thoracic vertebral body tethering, including thoracoscopy, when performed)
- 27278 (Arthrodesis, sacroiliac joint, percutaneous, with image guidance, including placement of intra-articular implant(s) (e.g. bone allograft[s], synthetic device[s]), without placement of transfixation device)
Note: New codes 27278 to the 27279 (Arthrodesis, sacroiliac joint, percutaneous or minimally invasive (indirect visualization), with image guidance, includes obtaining bone graft when performed, and placement of transfixing device) through 27286 (Arthrodesis, hip joint (including obtaining graft); with subtrochanteric osteotomy) have been created.
Revisions in 2024:
There are two revisions in 2024:
- Revised descriptor: 63685 (Insertion or replacement of spinal neurostimulator pulse generator or receiver, requiring pocket creation and connection between electrode array and pulse generator or receiver)
- Revised descriptor: 63688 (Revision or removal of implanted spinal neurostimulator pulse generator or receiver, with detachable connection to electrode array)
- Include the appropriate add-on bone graft code with fusion
The work of placing the bone graft is included in the arthrodesis/fusion codes and a bone graft code should be included when a fusion is performed. The coder has to examine the operative report to determine:
- Whether the bone graft was an allograft or an autograft, and
- Whether it was a morselized (bits or pieces) or structural (wedge or chunk) bone
Bone graft codes commonly-used as add-on in spine surgery include:
- Allograft (donor bone): +20930 (morselized), 20931 (structural)
- Autograft (patient’s bone): +20936, +20937 (morselized), +20938 (structural)
- Determine if hardware or instrumentation was used
The operative note should mention whether instrumentation was used in the fusion or not; if yes, the documentation should show where the instrument was used, and whether it was non-segmental, segmental, or intervertebral. Knowledge about the following is necessary to code instrumentation correctly:
- If the spacer is made from titanium, PEEK or bone
- If the surgeon used a standalone cage (includes built-in hardware to anchor the device)
- Whether the implant has a separate plate and screws (these require additional CPT codes)
- Whether it is a first-time implant, removal or revision surgery
The relevant CPT codes in this context are:
- Non-segmental instrumentation (+22840, +22836, +22837, and +22838) Posterior non-segmental instrumentation (e.g. Harrington rod technique, pedicle fixation across 1 interspace, atlantoaxial transarticular screw fixation, sublaminar wiring at C1, facet screw fixation) (List separately in addition to code for primary procedure)
- Posterior segmental instrumentation (22842, +22844) as “pedical fixation at each end of the construct and at least one additional interposed bony attachment,” meaning at least three points of attachment on the spine
- Anterior instrumentation codes (+22845, +22847) are based on the number of vertebral segments the hardware (typically, a plate) spans
- Intervertebral instrumentation (22853) Insertion of interbody biomechanical device(s) (e.g. synthetic cage, mesh) with integral anterior instrumentation for device anchoring (e.g. screws, flanges), when performed, to intervertebral disc space in conjunction with interbody arthrodesis, each interspace (List separately in addition to code for primary procedure)
Point to note:
AAPC cautions that as instrumentation codes are add-on codes, they should not be reported with modifier 62.
- Better management of denials
A clear understanding of why claims are denied is critical to identify and address issues in ASC revenue cycles. Often, reasons for denials could be simple billing mistakes such as demographic errors, incomplete claim submission and invalid modifiers or diagnosis codes. New documentation strategies can be implemented only by analyzing claim denials.
- Stay up-to-date with changes in medical policy
Billing policies vary with the choice of carriers. The methodology and efficiency of reimbursement for pain management procedures has drastically changed over the past few years. Follow the routine documentation procedures that have been effective in the past, but now result in denials. Your medical coding team must be aware of the differences and updates to each policy’s requirements. The team must also keep track of the coding changes and updates such as which codes have been deleted or replaced, as payers will reject the claim if you use an outdated code.
For proper CPT code assignment for spinal procedures, the operative note has to support the CPT code selection as well as postoperative diagnosis. It should also support medical necessity for a given procedure or service. Partnering with a pain management medical coding company with a team of experienced AAPC-certified coders who stay updated on the latest billing and coding guidelines as well as changes in payers’ rules can drive accurate and timely submission of claims and optimal reimbursement.
Let us handle your medical coding needs, ensuring compliance and efficiency every step of the way.
Maximize reimbursement with us




