Assigning correct codes is crucial. A growing number of practices are choosing to outsource this responsibility to a professional medical coding company. One reason for this is the national shortage of medical coders. In 2023, the American Medical Association reported that studies show there’s a 30% shortage of experienced coders across the country. Hiring and maintaining a team of in-house coders can be substantially more expensive than outsourcing this work. Partnering with a reliable provider will give you access to certified coders with experience specific to your practice or specialty, without the need for hiring and training new employees. So, how do you choose the right one for your practice?

Importance of Choosing a Reliable Coding Service
Converting procedures and services documented in medical records into the right medical codes ensures that patient records are accurate. Medical coding plays a key role in billing and mistakes can impact your revenue. Coding is challenging and only an experienced coding company can handle all types of medical scenarios and documentation. Choosing a reliable partner can help you avoid errors such as upcoding, undercoding, incorrect modifiers, and more. They’ll help you submit accurate claims, reducing chances of denials and delays, improving revenue cycle efficiency.
Criteria that make a Good Medical Coding Company
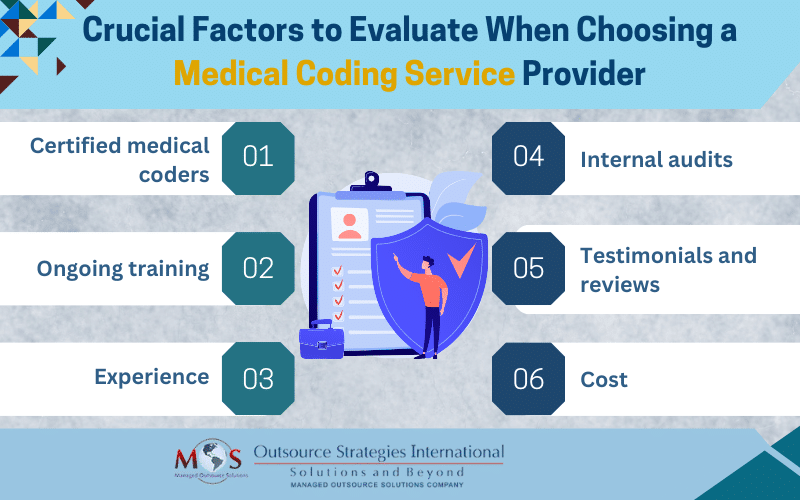
There are hundreds services out there and it can be overwhelming challenging to find the right one. Here are 6 things to look for before hiring a medical coding service:
Certified medical coders
It’s essential to partner with a company that has coders with certifications from authorities such as the American Academy of Professional Coders (AAPC) or the American Health Information Management Association (AHIMA). Examples of credentials to look for are CCS-P, CPC, COC, CRC, CPPM, CPCO, CDEO, and CPMA. Certified coders stay up to date with the latest ICD-10, CPT and HCPCS codes and National Correct Coding Initiative (NCCI) edits.
Experienced coders have a strong understanding of anatomy and physiology and can accurately translate diagnoses and procedures into highly specific codes. Make sure the company you choose has coders who are familiar with the requirements related to your specialty. Professional coders are also knowledgeable about current payer regulations and guidelines, which is crucial to assign the appropriate codes and submit accurate claims. They can also integrate their specialized knowledge, skills and experience with new technologies such as computer-assisted coding (CAC) and autonomous medical coding.
Ongoing training
A reliable company will ensure that its coders receive continuous training to stay well-informed and follow the latest regulations in the field. Such education and training programs can prepare coders to adapt to the continuously evolving landscape of healthcare and coding. Codes are revised and changed on a yearly basis and training is necessary to stay up to date.
Experience
It’s important to ask how long the company has been in business. Coders with a deep understanding of coding systems, terminology, and guidelines are less likely to make errors that can lead to claim denials. Experienced coders can also ensure compliance with legal and regulatory standards. Ultimately, their experience can promote accurate and faster claim submission, ensuring you receive appropriate reimbursement. Experience also helps with handling pressure and meeting deadlines.
Internal audits
Ask whether the company conducts internal audits to examine the payer reimbursement processes and federal regulations. By targeting high-risk areas, internal audits can identify specific issues or patterns in coding and documentation that might pose compliance risks. AAPC states that medical audits provide a system to:
- Review quality of care provided
- Educate providers on documentation guidelines
- Determine if organizational policies are current and effective
- Optimize revenue cycle management
- Ensure appropriate revenue is captured
- Defend against federal and payer audits, malpractice litigation, and health plan denials.
Testimonials and reviews
As with most other services, checking testimonials, industry recommendations, opinions of medical specialists, and reviews are important when choosing a medical coding company. Reliable companies have client testimonials easily findable on their website. Partner with the company that has the highest number of positive reviews, with focus on your specialty.
Consider cost
It’s important that you know how much you will be charged. Choose a company that offers rates that stays within your budget and has a pricing structure that meets your needs. Make sure there are no hidden charges. Outsourcing to reliable companies can help you cut 30-40% on your overhead.
New advancements in technology are helping increase efficiency and precision, adhere to standards, and optimize resource allocation. However, automation is always missing critical things like modifiers that can be used to get the claim paid. So, make sure to choose a company that has skilled certified coders as there is always a manual aspect to coding. These professionals continually advance their knowledge and expertise and stay up to date on changing codes and standards. Partnering with an expert can help you overcome the challenges of medical coding, streamline documentation processes, enhance patient care outcomes, and increase cash flow.