In-house Claim Management Is Difficult
Health insurance claims management is a pivotal aspect of running a successful medical practice, directly influencing the patient-provider relationship. The healthcare industry has undergone a tremendous transformation over the past few years, and the healthcare revenue cycle process has as well. Physicians and other professionals no longer have to do the tedious task of manual coding and claim submission for reimbursement since automation took over.
However, healthcare professionals need to focus on providing excellent patient care, so this administrative task of capturing payments through claim processing can be a taxing, burdensome and downright frustrating job on the providers. Between constant updates of regulations, denied and rejected claims, delayed payments and heavy workload, claim processing could lead to inefficient workflow and revenue leakage. To mitigate these difficulties, hiring a medical billing services provider would ensure faster claim resolution, improved patient satisfaction and seamless revenue flow. Claims management outsourcing is the practical way for providers to increase efficiency and revenue.
A successful claims management service provides many benefits. First of all, there is the immense financial impact. A process that ensures quick payment will result in reduced administrative costs, often brought about by these time-consuming claims application processes. It also filters down to the relationship the doctor has with the patient. Effective claims management makes the relationship better. Inappropriate payments from the health insurer can cause a negative impact on the relationship and the kind of care given.


Simplify your claims processing with our billing professionals and boost your revenue!
Why Claims Management Outsourcing Is Vital
Claim management companies are committed to managing everything that involves a claim including collecting data, verifying patient eligibility, filling submission, denial management and compliance with insurance and governmental rules and regulations. Outsourcing aids in optimizing the entire process to ensure patient retention, reduced claims, and timely payments. It also helps improve your practice’s cash flow and ROI.
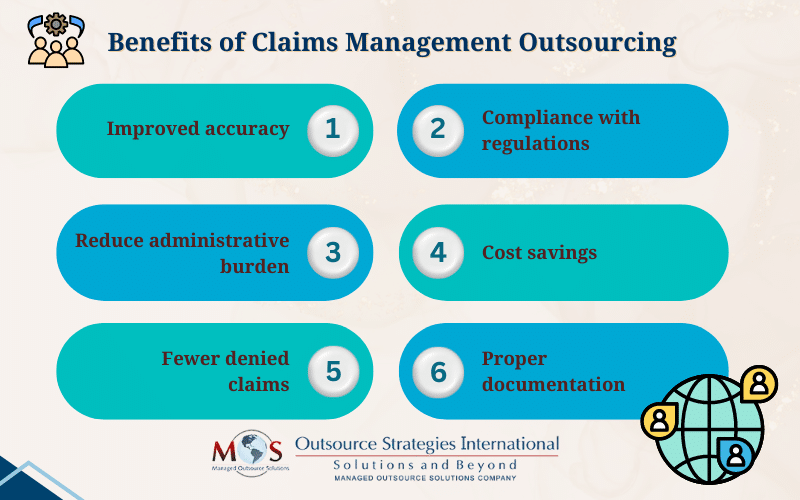
If you still have doubts regarding the use of hiring a claim management company for your medical practice, read the below list to find out the benefits of outsourcing.
- Improved accuracy
Claims processing is a time-consuming task and if not handled with meticulous effort and focus could lead to errors. Your medical practice’s staff, despite their best efforts, may not have the expertise needed in coding and billing. In this scenario, outsourcing to a medical billing company could be a game-changer for your practice.
Medical billing companies have a pool of professional staff knowledgeable and experienced in their respective fields to streamline the billing process. This ensures timely, accurate and complete claim submissions. The result is a well-regulated billing system that provides faster payments, less denied claims and increased cash flow to your practice.
- Compliance with regulations
As a medical professional your time and energy are primarily devoted to attending to your patient’s care and health. The claim filing procedure is a tiring, worrisome job, and you could end up spending time attending compliance seminars, webinars, going to meetings and studying the latest rules. All of these might take a toll on your health and the time for your practice, which could end up as lost revenue.
By hiring a claim management agency, you will always have a great team of skilled specialists at your disposal to give the responsibility of managing your claims. They provide guidance and ensure adherence to state and insurance payer’s regulations so your practice abides with ethical, safe and legal rules.
- Reduced administrative burden
By outsourcing claim processing to a trusted agency, you reduce the amount of administrative work and the time it takes to complete them from the hands of your staff and yourself onto the hands of skilled workers. This allows you to focus mainly on giving exceptional patient care and more time and flexibility for your staff to focus on critical tasks.
Deadlines, denied claims, unpaid benefits and huge workload can negatively impact on your practice’s environment. When you outsource, you create a productive workflow thereby increasing your practice’s financial health as well.
- Cost savings
While it may seem like an added expense at first glance, you actually safeguard the financial health of your practice by outsourcing. Overhead costs associated with hiring and training in-house staff, additional cost of learning, and staying updated with regulatory changes and any other technical repair costs as well can be reduced when you partner with a management company.
Moreover, if insurance companies intentionally delay the payments deserved, claims management companies have the in depth experience and resources required for paperwork of Medicare, Medicaid and other private insurance companies as well. They can also file a complaint on your behalf as well if payers purposely refuse the claim submission.
- Fewer denied claims
Just the way you are the specialist that people visit for the diagnosis and treatment of health related matters, a claims management agency is the specialist for claims processing. They handle the process from start to finish and know exactly what to do to avoid claim denials. In the event of a claim denial, they will correct the errors and resubmit the claim and if there’s need for an appeal, they can file one on your behalf.
With the advent of electronic claim submission, claims management companies have access to advanced, sophisticated software tools that help prevent human-error and enhance submission rate. Timely submissions accelerate cash flow and help you maintain successful practice.
- Proper documentation
Partnering with an experienced medical claims processing company can go a long way in improving your practice revenue. You need to establish proper communication with your medical coding team to ensure proper documentation, which is crucial to maximize your reimbursement benefits.
Here are some tips to ensure accurate documentation for efficient management of your claims
Provide detailed procedure specifications – When it comes to making surgical notes, you should document the exact details such as identifying the surgical approach, procedures performed, and any unusual occurrence during the surgery. For instance, ICD-10 has greatly increased the specificity for selecting codes. While some codes are based on laterality, for instance, right ear, left ear, bilateral ear and unspecified ear, other codes are selected on the basis of whether the condition is a first occurrence or a re-occurrence. So if you perform a complicated surgical procedure, you should specify every detail in your surgical notes so that the correct codes can be assigned.
Documentation of time – Many codes are based on the time the physician spends with the patient as for instance, critical care which comes under time-based codes (99291-99292). For codes based on time, you have to document the total time spent which includes the time on the face to face with the patient and floor time with the patient and/or family member, time spent on reviewing diagnostic tests, and discussions with other providers involved in the treatment. A description or summary of the counseling/ coordination of care has to be provided with the claim along with the specific time spent on these activities.
Beware of EHR documentation shortcuts – EHRs have simplified documentation and help physicians save time by cutting and pasting information from a previous patient or selecting from a drop-down menu. Such shortcuts can be justified to some extent, but you should remember that progress notes are important to justify continued hospitalization. Insurance companies would pay only if they are convinced that the services were medically necessary and your notes should indicate this clearly.
How Can EHR Reduce Administrative Costs?
Cost savings due to EHR system can be attributed to the digitalization of medical records which facilitates accurate and faster exchange of data between internal systems, teams and departments across a hospital, which can be done in real-time. This streamlines the documentation, billing and coding processes thereby eliminating errors and saving your practice’s administrative costs.
The EHR market size is expected to increase by $32.27 billion, growing at a CAGR of 12.91% from 2022 to 2027 and the top contributor to the global market is United States with 41%. EHR regulations are standardized under the Office of National Coordinator for Health Information Technology and the adoption of electronic health record (EHR) is encouraged by the government, who linked their usage to medical reimbursement. The failure of it on any medical practice’s part results in penalties starting from 2024.
The ONC encourages the health sector to implement standardized APIs that when integrated with EHR technology, improves communication between IT system and smartphone application that create and store medical information. This enables quick access and exchange of the medical information stored among multiple groups.
EHRs themselves may not help save money, it is required to devise a strategy that includes both EHR and healthcare delivery methods for actual cost savings. If doctors’ offices implement servers and other facilities for maintaining electronic health records in-house, their costs will add up. The better option is outsourcing medical billing and health record maintenance. A professional medical billing company can launch EHRs on behalf of doctors’ offices, monitor all healthcare delivery methods and manage the billing properly. This way, the company can take up the entire responsibility of billing staffs and reduce the administrative costs in physicians’ offices. This will eventually reduce the amount spent for patients each month.
It is understandably a drain on the healthcare practice’s resources to assign staff exclusively for claims management service. Though it is an important task, claims management is a non-core responsibility, something that will prove to be too intimidating for small practices to handle by themselves. This is where a medical billing and coding company comes in.
A medical billing and coding company caters to all these requirements of healthcare practices. It is familiar with all the AMA and CMS-recommended procedures and can take over claims management tasks for hospitals, nursing homes, rehabilitation centers, and individual physician practices.
Outsourcing claims management ensures that healthcare practices get paid promptly and also that they cut costs and save precious resources.