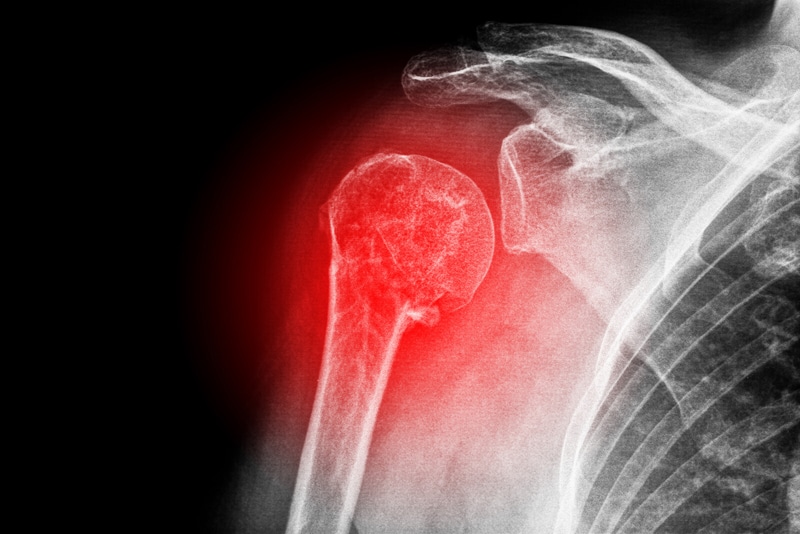
Osteoporosis is a systemic condition, meaning that all bones of the musculoskeletal system are affected. As this disease is characterized by low bone mass with microarchitectural disruption and skeletal fragility, there is an increased risk of fracture, particularly at the spine, hip, wrist, humerus, and pelvis. Documenting these osteoporotic fractures for claim submission and reimbursement requires a better understanding of the coding guidelines for coders. Physicians could also consider accurate medical coding services provided by an experienced firm.
Though we have discussed earlier about documenting Osteoporosis with ICD-10 coding, here are some more tips that orthopedic coders can consider.
Check whether the fracture is traumatic or pathologic
Check the physician’s documents to know whether the fracture is traumatic or pathologic (non-traumatic). A traumatic fracture is caused by accidents, falls or other kinds of force, while pathologic (non-traumatic) fractures are caused by diseases like osteoporosis. However, in most cases physicians don’t always specify the fracture clearly as open or closed. Instead, for a closed fracture they may use terms such as Comminuted, Depressed, Elevated, Fissured, Greenstick, Impacted, Linear, Simple, Slipped epiphysis and Spiral. For open fracture types, terms used include compound, infected, missile, puncture and with foreign body.
Other important information to include when reporting a fracture is – “site of the fracture”. This includes not only which bone is broken, but also the specific location of the fracture on the bone. Coders must include details such as “distal end” or “proximal end”.
Is the fracture “current” or not
If the patient has a current pathological fracture at the time of the encounter, use the codes from M80- series. The code should be selected based on the site of the fracture, not the location of the osteoporosis. A code from category M80, not a traumatic fracture code, should be used for any patient with known osteoporosis who suffers a fracture, even if the patient had a minor fall or trauma, if that fall or trauma would not usually break a normal, healthy bone.
- M80 Osteoporosis with current pathological fracture
- M80.0 Age-related osteoporosis with current pathological fracture
- M80.00 Age-related osteoporosis with current pathological fracture, unspecified site
- M80.01 Age-related osteoporosis with current pathological fracture, shoulder
- M80.011 Age-related osteoporosis with current pathological fracture, right shoulder
- M80.012 Age-related osteoporosis with current pathological fracture, left shoulder
- M80.019 Age-related osteoporosis with current pathological fracture, unspecified shoulder
- M80.022 Age-related osteoporosis with current pathologic fracture, left humerus
- M80.041 Age-related osteoporosis with current pathologic fracture, right hand
- M80.871 Other osteoporosis with current pathologic fracture, right ankle and foot
Osteoporosis without Current Pathological Fracture
If the patient does not have a current pathological fracture, a code from M81-series should be selected, even if the patient had a pathological fracture in the past.
The codes in this series include –
- M81 Osteoporosis without current pathological fracture
- M81.0 Age-related osteoporosis without current pathological fracture
- M81.6 Localized osteoporosis [Lequesne]
- M81.8 Other osteoporosis without current pathological fracture
If there’s no current fracture, but there was one in the past, you should report using
- Z87.310 Personal history of (healed) osteoporosis fracture
If an osteoporosis patient fractures a bone after a minor trauma, use a code from category M80, which is not a traumatic fracture code. Make sure that the documentation clearly states that you are dealing with an osteoporotic pathologic fracture. If the documentation is not clear, query the provider.
Use the right seventh character with code
The seventh character is crucial to identify the type of encounter for which the patient is being seen. Without the seventh character, the code will be considered invalid and the claim will be rejected. If the cause of the patient’s osteoporosis is something other than age, capture it with a code from M80.8- (Other osteoporosis with current pathological fracture).
Make sure to add one of the following seventh characters to each code:
- A: Initial encounter for fracture
- D: Subsequent encounter for fracture with routine healing
- G: Subsequent encounter for fracture with delayed healing
- K: Subsequent encounter for fracture with nonunion
- P: Subsequent encounter for fracture with malnutrition
- S: Sequela
Seventh character A or initial encounter should be reported while the patient is receiving active treatment for the injury such as surgical treatment, ED encounter or evaluation and treatment by a new physician. At the same time, other characters including D, G, K, and P denote encounters such as cast change or removal, removal of external or internal fixation device, medication adjustment or other aftercare and follow-up visits.
It is also recommended not to report ICD-10-CM aftercare Z codes for aftercare for injuries. To report aftercare of an injury, assign the acute injury code with the appropriate seventh character for subsequent encounter. Medical billing and coding outsourcing is a great option for busy orthopedists as well as other specialists to get their claim submission tasks done with accurate codes.