Anesthesia is a complex branch of service that comes with its own unique set of standards and procedures. Therefore, it’s no surprise that anesthesia has its own specialized billing process. The intricate work of an anesthesiologist begins during the pre-surgical phase where they gather information to create an anesthesia plan specific to each patient. They then monitor their pain to provide the appropriate dosage during the surgery and supervise the patient’s condition post-surgery.
Anesthesia has a branch of billing that revolves around unique requirements and regulations. This is a daunting task unlike other billing processes since anesthesiologists do not get paid based on the fee-for-service model but rather on a system containing base units, time units, modifier units, and other additional procedures.
Your medical practice has to navigate the complicated process of anesthesia medical billing and coding with strategies to circumvent denials and ensure timely reimbursement.

Challenges in Anesthesia Billing
-
- Complex billing
Anesthesia billing is different from standard billing processes as it is based on charge capture which is calculated on the level of difficulty of the procedure and the time taken. Complexities include the diverse nature and duration of procedures performed, differentiating between medical direction and medical supervision, proper use of modifiers, accurate documentation, and intricate coding of each service and stringent compliance with standard regulation. The basics of anesthesia charge calculation criteria are:
-
-
- Difficulty of the procedure performed
- Time
- Modifying factors (such as patient’s health)
-
The general formula for calculating anesthesia charges is:
(Base units + Time units + Modifying units) x Conversion factor = Anesthesia charge
-
- Base Units – Each anesthesia procedure has a unique code with a corresponding base unit value. As the complexity increases, so does the base unit.
- Time units – Time units are determined using the total time in minutes actually spent performing the procedure. A time unit is 15 minutes.
- Modifying units – Modifying units prevent duplicate billing and encompass factors like emergencies or certain conditions in patient’s health.
- Conversion factor – This is the cost assigned to each unit and varies according to the provider’s location.
-
- Anesthesia coding concerns
Inaccurate coding is one of the top issues that affects anesthesia RCM. Anesthesiologists need to determine how to properly code for their time spent in surgery and choose the method that best describes the intensity of service provided. Providers have to figure out which of the codes applies to an individual case, which can be really challenging as there are over 13,000 anesthesia codes. Moreover, anesthesiology codes are much more complex than that of other specialties, and providers need to be vigilant to avoid coding errors. Here are the common anesthesia coding factors to note:
-
- Map the codes – Identify the CPT codes for the surgery performed to map with the respective anesthetic CPT/ASA codes. Make sure that you master the procedure codes issued by HIPAA and HCPCS as they reflect the complexity of the surgical procedure and the type of anesthetic services you administered, including the specific codes for local, moderate, general, regional, and monitored anesthesia care.
- Report the right codes – The right CPT and HCPCS codes and modifiers provide information about the service and how it was performed. ICD-10 codes show why a service was performed, that is, they establish medical necessity and also determine if the circumstances in which the service was provided are in accordance with the payer’s coverage policies. ICD-10 codes change when the fiscal year begins on October 1, while CPT code updates take effect with the start of the calendar year. Medical billing and coding service providers need to stay up-to-date on annual coding changes.
- Time-based billing – Since anesthesia services are billed on the basis of the duration of the service given, it’s important to track and understand the rules for time-based billing. You must record the complete administration time of the service given starting from pre-surgical sedation until the patient is admitted to the post-anesthesia care unit. This is required to calculate the reimbursement rate by insurance companies.
- For multiple procedures, bill the procedure with the highest base value: Some ASA codes include multiple areas in their description and have higher base units. When working in multiple areas of the spine and abdomen, an anesthesiologist can avoid under-billing their services by using codes with higher base units.
- Documentation difficulties A large portion of an anesthesia provider’s job involves documenting multiple phases such as:
- Pre-operative evaluation
- Intraoperative/procedural anesthesia
- Post-operative care
To submit accurate anesthesia claims, you need a comprehensive record capturing the base, time and other modifiers. Any inaccuracy can lead to various issues including billing errors, claim denials, legal repercussions, and loss of revenue.
Procedures cancelled before induction must be reported using the correct evaluation and management code. The reason why the case was cancelled must be given, such as cancellation due to equipment failure. Procedures cancelled after induction should be reported with the appropriate modifier plus time. If the payer does not accept a modifier, these cases can be billed using the correct anesthesia code with the full base units for the procedure that was scheduled, plus total time that is documented on the anesthesia record. The documentation should clearly specify the reason for the cancellation.
-
- Frequent regulatory changes
Anesthesia billing must be done keeping in mind the applicable coding guidelines and federal/state regulations related to Medicare and Medicaid. Insurance companies have their own unique set of rules and policies as well that differ from one another. As an anesthetic professional, staying updated and adhering to these constant changes is vital for you to avoid claim rejection or delayed payments.
-
- Pre-authorization Needs
An anesthesiologist has the responsibility to obtain a pre-authorization from insurance providers if it is required to do so before providing the treatment. So, check with your patient’s payer’s policies before the appointment.
-
- Use of modifiers
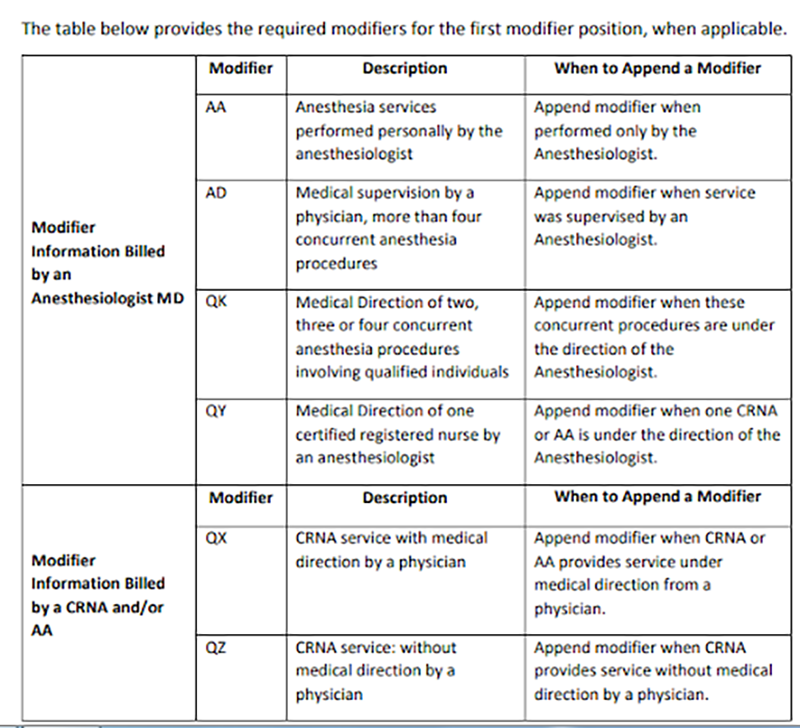
There are several modifiers in anesthesia and providers need to know how to use correctly. Modifiers signifying physical status, age and emergency factors may be added to the procedure codes. The total number of units is then multiplied by a conversion value to create a total charge for the procedure. When billers are not fully aware of modifier usage, the result can be inappropriate billing and overpayments. There are two broad categories of anesthesia modifiers- pricing modifiers and informational modifiers.
Pricing modifiers are assigned based on the number of providers and their roles in the anesthesia service. Pricing modifiers must be submitted in the first position to indicate whether the service was personally performed, medically directed, or medically supervised.
Medical coders should be knowledgeable of the various modifiers and how to use them correctly to ensure proper claims payment.
Key modifiers, as explained by BlueCross BlueShield of Texas, are as below:
Informational modifiers are placed in the second modifier position and are critical for the billing process, though they do not directly affect reimbursement. For e.g. QS – Monitored anesthesia care service. (Report with anesthesia CPT codes along with actual anesthesia time). Another set of informational modifiers are those used to indicate the patient’s physical status during the anesthesia procedure, for e.g. P1 – A normal healthy patient, P2 – A patient with mild systemic disease, etc.
-
- Denial management
An effective claims management team is an indispensable part of revenue cycle management in any medical practice. As the majority of your time and energy is used for patient care and other clinical, administrative tasks, claims follow-up might not be at the top of your list. However, this single action is instrumental in deterring the financial performance of your practice. Insurance companies are vigilant while scrutinizing and evaluating your submissions, so even a single mistake on your part could lead to your claim being denied. To successfully navigate and identify the reason for your claim denials, you need an expert in handling denied claims. By outsourcing your denial management to an experienced medical billing company, you can understand the root cause of claim denials and prompt payments.
Anesthesiology CPT Codes 2024
With reimbursement based on value, collaborative care, and new technologies impacting anesthesiology, most practices rely on anesthesiology medical billing services for accurate claim submission. Each year brings about expectations of changes in codes and billing requirements in the anesthesia specialty. Partnering with an anesthesiology medical coding company is the practical option to maintain compliance with insurance providers, ensure correct coding, and submit accurate claims.
The Anesthesia CPT (Current Procedural Terminology) code range is from 00100 to 01999.
- Head 00100-00222
- Neck 00300-00352
- Thorax (chest wall and shoulder girdle) 00400-00474
- Intrathoracic 00500-00580
- Spine and Spinal Cord 00600-00670
- Upper Abdomen 00700-00797
- Lower Abdomen 00800-00882
- Perineum 00902-00952
- Pelvis (except hip) 01112-01173
- Upper Leg (except knee) 01200-01274
- Knee and Popliteal Area 01320-01444
- Lower Leg (below knee, including ankle and foot) 01462-01522
- Shoulder and Axilla 01610-01680
- Upper Arm and Elbow 01710-01782
- Forearm, Wrist and Hand 01810-01860
- Radiological Procedure 01916-01942
- Burn Excisions or Debridement 01951-01953
- Obstetric 01958-01969
- Other Procedure 01990-01999
Anesthesia billing is unique due to its intricate coding challenges, time-based billing and ever-changing regulations. To navigate the complex process of billing for anesthesia, outsourcing to a specialized billing company provides many benefits including improved billing and coding accuracy, reduced claim denials, enhanced compliance with anesthesia-specific payers and governmental regulations, streamlined workflow and maximum reimbursement.