Effective denial management in medical billing is crucial for ensuring timely reimbursements and minimizing financial disruption for both healthcare providers and patients. A denial occurs when a healthcare insurance company reviews a claim and refuses to provide payment for the requested services. Unlike rejections that occur as a result of errors or discrepancies in the claims data, denials occur due to reasons like lack of medical necessity, incorrect coding, or insufficient documentation. Medical billing denials pose significant challenges to healthcare providers, leading to increased administrative hassles, delayed payments and eventually, potential financial losses. Outsourced medical billing and coding services is an effective option to handle denials proactively and maintain a positive revenue cycle.
This post will help you understand the differences between claim denials and rejections, explore the common types and causes of denials, and provide tips to prevent them.
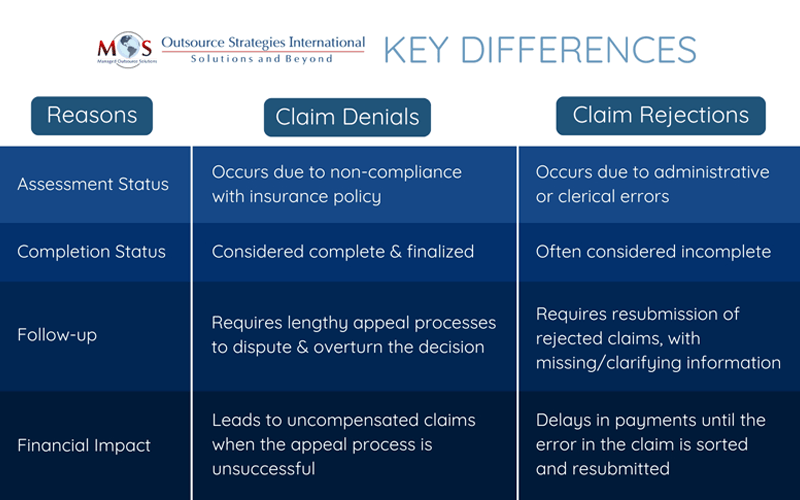
Claim Denial vs. Claim Rejection
Denial and rejection are two ways an insurer responds when they decide not to pay a claim. As a healthcare provider, it is important to understand the nuances between a claim denial and rejection to accurately address them and get paid promptly. Let’s examine the reasons for claim denials and rejections and the steps you can take to mitigate these risks.
- Claim Denials: Denials usually happen after the claim goes through adjudication and processing. It occurs as a result of non-compliance with regard to the payer’s policies. Common reasons for denial include incomplete documentation and coverage constraints. For instance, a claim can be denied if the procedure is considered elective and not medically necessary.Claim denials are challenging as the insurer has processed the claim and identified that it does not qualify for payment. This means the claim must go through an appeals process to overturn the decision, which can be difficult and time-consuming.
- Claim Rejections: Rejections occur at the primary stage (initial review), when the insurer identifies errors or discrepancies in the documentation. These errors can range from invalid procedure/diagnosis codes, incorrect patient demographics to incorrect payer information.
Unlike denials, rejections can be often corrected and resubmitted without going through the lengthy appeal process.A professional medical billing company specializes in managing claim denials and rejections to ensure healthcare providers maintain a healthy revenue cycle. They help providers identify the root causes of denials and rejections, streamline the claims process, appeal denied claims, and implement proactive measures to prevent future errors
What are the Common Causes of Claim Denials?
There are several reasons that lead to claim denials and understanding them can help providers identify and fix issues expeditiously.
- Incomplete Documentation: Missing information or incomplete clinical records can lead to denials.
- Coverage Exclusions: Insurer will not be covering procedures that are outside the patient’s insurance plan.
- Care Decline: The care was deemed to be not medically relevant for the said treatment or diagnosis.
- Preauthorization Issues: Treatments that require prior authorization weren’t submitted or were denied.
- Coding Errors: Errors that occur in diagnosis/medical coding (CPT, ICD, or HCPCS) can trigger denials.
- Late Submissions: Claims that were submitted beyond the insurer’s deadline will be denied.
The Financial Impact of Claim Denials
Industry reports suggest that nearly 20 percent of all claims are denied. Up to 65 percent of denied claims are never resubmitted, according to the Healthcare Financial Management Association (HFMA). This leads to heavy financial losses with for reaching consequences for the revenue cycle of a healthcare practice. Frequent change in payer policies and regulations add to the problem.
A streamlined denial management system can help providers prevent or minimize denials and boost overall cash flow.
What are the Best Practices to Prevent Claim Denials?
- Defensive Eligibility Checks: Make sure to verify insurance coverage, benefits, and policy details in advance, at the time of the appointment scheduling.
- Accurate Documentation: Ensure all necessary clinical records, including lab results and physician notes are correct.
- Error-free Medical Coding: Bring in expert medical coders to ensure correct procedure and diagnosis coding that meets payer guidelines. They will be updated on changes to coding standards like ICD and CPT.
- Prior Authorizations: Check pre-approval for procedures, especially for costly or specialized procedures.
- Prompt Filing: Processes should be established to ensure claims are submitted well before the insurance company’s deadlines.
- Incorporate Technology: Invest in billing software to identify errors before submission and properly track claim status.
Steps to Resolve Denied Claims
Addressing denials is not a straightforward process, but if you follow a systematic approach, you might be able to turn the decision in your favor.
- Analyze the Reason for Denial: Identify the reason by evaluating the insurer’s explanation of benefits (EOB) to get around the issue.
- Fix Errors: Once the issue has been identified, work towards fixing the errors, if they are coding errors or missing documentation.
- Appeal the Denial: If the issue is beyond any administrative errors (policy disputes), then consider filing an appeal with proper documentation and justification.
- Trend Monitoring: Using billing software, track denial patterns to identify issues and use it to improve processes for upcoming claims.
Partner with an Expert
Partnering with a professional outsourcing company providing medical coding services can reduce claim denials and improve the revenue cycle.
At OSI, our experienced team is up to date on coding changes and insurance rules and policies, which helps ensure accurate claim submission. With timely review of denial and audit data through advanced medical billing software and ongoing communication with payers, an expert can help you minimize errors that lead to denials.
Losing Revenue to Claim Denials?
Take control of your revenue cycle with our state-of-the-art medical billing services. Partner with us for minimized denials and maximized reimbursements!




