Dental insurance verification and reimbursement for core buildups can be challenging. Dental offices and dental billing companies must be up to date with CDT codes and payer guidelines to ensure accurate claim submission. Let’s first take a look at the difference between post and core buildup.
What’s the Difference between Post and Core Buildup?
A post and core buildup are closely related but serve different purposes. In some cases, both post and core buildup are needed but in others only core may be used. Post is recommended only in cases in which the tooth structure is highly damaged or more than 50% of the original structure is removed.
Core buildup with pins: Traditionally, metal pins were used for core buildup by removing decayed areas of tooth and reinforcing the teeth with metal or fiber pins into its structure.
Core buildup with post: Core buildup with post is performed after root canal when there are not enough teeth left intact to keep the crown in place. A post made of thin metal or fiberglass is inserted into the tooth’s root canal space and this helps to retain the tooth’s core. The post acts as an anchor for the subsequent restoration crown which is bonded to the core material.
D2950 – Buildup versus D2949 – Foundation
Dental insurance reimbursement for core buildups is often challenging. Many dentists routinely remove all existing filling from a tooth when they do a crown preparation. This can leave several irregularities, undercuts, and divots. The dentist further places a material to fill in these irregularities, so that the final shape of the prepared tooth is “ideal”. This is often confused with a D2950 buildup, which is a similar procedure but is done for a very different reason.
D2950 – Core Buildup, Including Any Pins
- Descriptor was changed in CDT 2014 – it was simplified to clarify the purpose and intent of a buildup.
- CDT 2014 descriptor – “Refers to building up of coronal structure when there is insufficient retention for a separate extra coronal restorative procedure.”
- There is no longer a reference to “tooth strength” in the descriptor.
- The purpose of a buildup is to help hold the crown on when there is not enough tooth structure left. In other words, if a buildup is not done, then the crown would not stay on.
- The CDT 2014 descriptor also states “A core buildup is not a filler to eliminate any undercut, box form, or concave irregularity in a preparation.”
- It is not appropriate to use this code for fillers or bases (included in the restorative procedure itself).
D2949 – Restorative Foundation for an Indirect Restoration
- Code implemented in CDT 2014.
- CDT 2014 descriptor: “Placement of restorative material to yield a more ideal form, including elimination of undercuts.”
- The procedure involves placing a restorative material in the tooth for purposes other than helping the new crown to stay. These purposes include – blocking out undercuts, eliminating a box form, filling in voids in the prep, filling in a concavity and making the shape of the prepped tooth more ideal in contour.
- This procedure is what many dentists were previously doing, but incorrectly submitting as a D2950 buildup.
Some of the important points to note here are –
- There is a difference between a buildup and a base, liner, or foundation.
- Placing a restorative material in order to protect pulp is not a buildup.
- Placing a restorative material in order to idealize the prep is not a buildup.
- Placing a restorative material in order to eliminate undercuts is not a buildup.
- Placing a restorative material in order to bond tooth structure, cusps, or cracks together is not a buildup.
- When there is sufficient tooth to retain a crown, then the shape or size of the crown prep doesn’t matter; the restorative material placed is not a buildup.
Core Buildup Post and Core and Pin Retention – Coverage Guidelines
Post and Core
Post and core are used for the following:
- For teeth with significant loss of coronal tooth structure in endodontically treated teeth in which insufficient tooth structure remains to adequately retain an Indirect Restoration
- For Posts when there is inadequate remaining tooth structure to support a core
Post and core are not used for teeth with short roots. A post is not used when anatomic features are available to retain the core (e.g. when canals and pulp chamber can retain a core).
Pin Retention
Pin retention is used for teeth with significant loss of coronal tooth structure to allow retention of a direct restoration.
Pin retention is not used for the following:
- For restoration of teeth with significant malocclusion
- If the tooth cannot be properly restored with a direct restoration due to anatomic or functional considerations
Post Removal
Post removal is used for the following:
- When there has been loss of adequate retention
- In the case of fracture of tooth and/or post and core
- When there is recurrent caries associated with post and core
- When access is needed to the root canal system for non-surgical endodontics
- When the tooth has a reasonable long-term prognosis for a new restoration
Coverage Limitations
- Pin retention and post and core can be subject to a 12-month waiting period
- Pin retention is limited to 2 Pins per tooth
- Re-cementation of post and core is limited to those performed more than 12 months after the initial insertion
Reimbursement Challenges
The code used for core buildup D2950, is often misused by many dental practices. The existence of a CDT code does not necessarily mean that the procedure is covered or reimbursed by a dental benefits plan. This restorative procedure is typically recommended when:
- Teeth that do not have enough tooth structure to support a crown, as 60% or more of the tooth is missing in these instances.
- The remaining tooth preparation is less than 2.0 mm from the crestal bone
As this procedure is performed before restoring a tooth with crown, the benefit plan may get bundled with the crown procedure plan. Bundling separate procedures for the purpose of limiting benefits is against the norms of ADA. So when insurance providers decide to bundle these procedures, the total fee should be the sum of the fee for the core buildup and the crown with appropriate benefits. The parameters of dental plans may create confusion for the patients so it is incumbent for dental professionals to inform them beforehand to avail benefits and prepare for any out-of-coverage payments.
To minimize claim denials for core buildups, documentation of the condition that resulted in the buildup should be provided in the initial claim submission. This must essentially include documentation indicating that the tooth was broken down to the extent that a buildup was necessary for crown retention. Also, including Pre and Post Op x-rays can increase the chances of claim approval.
Health insurance payers may deny payment for the following reasons:
- A cracked tooth. Cracked tooth syndrome occurs when a tooth has a crack that is too small to show up on X-rays or is under the gum and challenging to identify. Claims for cracked tooth syndrome often get denied because radiographs do not show the cracks or make it clearly visible.
- Some dental plans cover crowns when the teeth are broken down and have extensive structural damage (due to dental disease or accidental injury). However, if the third-party payer doesn’t see evidence of that, the claim may be denied.
- Claims may also be denied if the dental plan’s consultant indicates that the tooth has a poor prognosis. In addition, claims for abrasion and attrition are typically denied.
Knowing when to bill for a core build up has proved to be somewhat challenging for dentists. As CDT codes are subject to frequent changes (which are often difficult to understand), billing and coding for various dental procedures, such as the D2950, and getting claims approved can also be quite complex. Claim denials can have a significant impact on patients and dentists. Dental practices, in such situations, can rely on outsourced dental billing services to overcome these challenges. It is very important for dental practices to understand the common billing and coding points that can largely affect their bottom-line.
Even in the face of denials of claims for core buildups, dentists need to treat patients with appropriate care regardless of the patient’s insurance coverage. The dentist must explain in detail why a specific procedure may not be covered before initiating the treatment procedure, so as to avoid a potential large unexpected bill on the patient’s part in the future.


Our team of experts dedicated to dental billing and coding has the right solutions for every challenge!
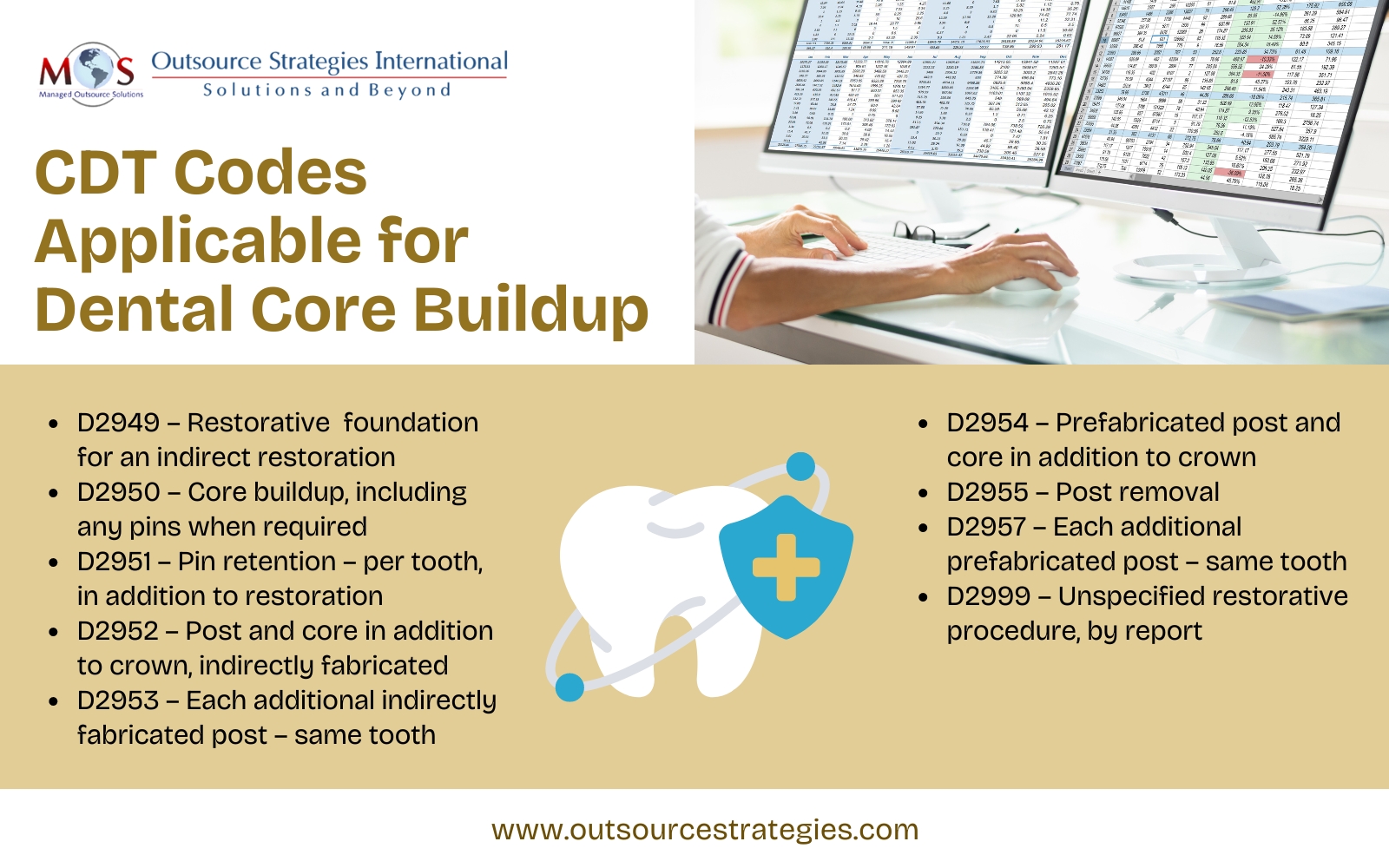
Applicable CDT Codes
Dental billing services provided by an experienced dental billing company are a great support for practices to meet their billing and claim submission requirements. Such companies will provide the services of skilled AAPC-certified coders and expert billing specialists who can ensure that your practice has fewer unresolved dental claims.