Dermatology practices must adhere to the latest dermatology CPT coding and billing guidelines for accurate reimbursement and compliance. Accurate clinical documentation of the procedures along with the relevant medical codes is necessary to submit medical claims for the dermatological services rendered. Providers of dermatology medical billing services will carefully evaluate the documentation and pull out everything related to the procedures to apply the right codes and modifiers.
Though all medical specialties face claim denials and audits, these concerns are more common in dermatology. Dermatology billing and coding requires thorough reporting, detailed information on procedures completed, and must follow multiple procedure rules, which can lead to billing and coding errors. Staying abreast of the latest trends – such as changing codes, billing rules, documentation requirements, and payment methods, is crucial for success with dermatology medical billing. Outsourced dermatology medical billing and coding services is a practical solution to stay current on medical codes and billing rules and ensure proper payment for your services.
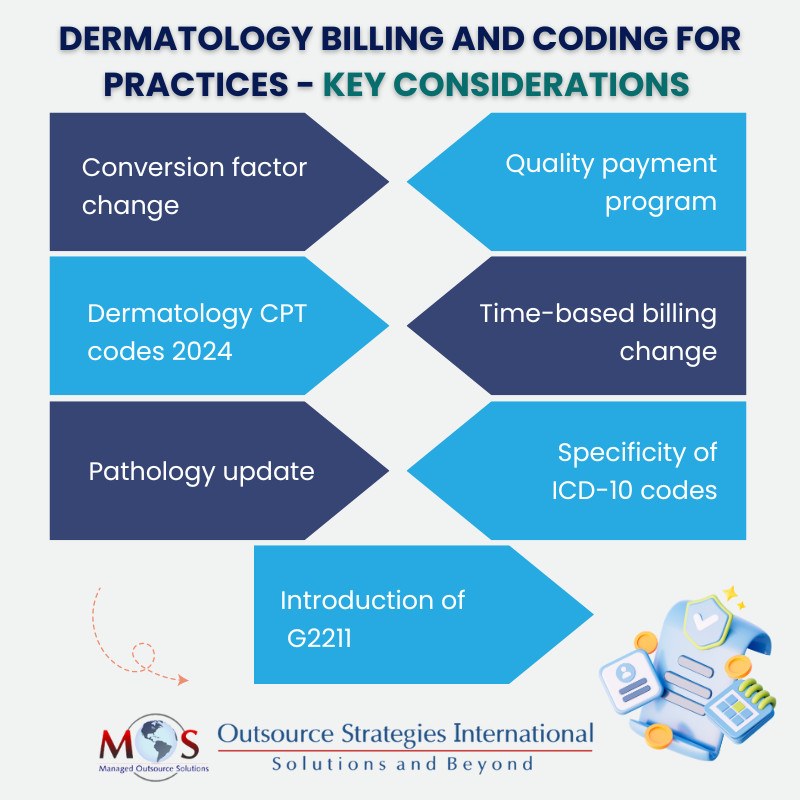
Let’s check out the top dermatology billing trends that medical practices need to pay attention to:
Conversion Factor Change
The new policy for the calendar year 2025 Medicare Physician Fee Schedule (PFS) set by CMS proposes a policy change to the conversion factor at $32.36, a decrease of $0.93 (or 2.80%) from the present conversion factor of $33.29. Although dermatology has multiple revenue streams, this rate change may negatively impact the ability of dermatology practices to provide quality patient care.
In a study presented at the American College of Mohs Surgery (ACMS) ’24 annual meeting, it was found that payment rates in Medicare decreased for several dermatology procedures. The CPT codes for various dermatological procedures were analyzed to find declines in reimbursement rates when compared with their inflation-adjusted values. CPT codes such as 17311 and 1700 showed a decrease of 46% over the period of past 18 years, when in fact they should actually have increased by 42% and 41%, respectively.
Our dermatology billing and coding services streamline your RCM process for efficient reimbursement flow!
Quality Payment Program
In the same proposed rule, CMS through the Quality Payment Program (QPP) aims to strengthen the Merit-based Incentive Payment System (MIPS). As part of this program, six new MIPS Value Pathways (MVPs) provisions are included, one of them being dermatology. Under MIPS, dermatologists would be eligible for value-based care reimbursement by evaluating performance in 4 separate areas of quality measures – quality, improvement activities, promoting interoperability, and cost.
Dermatology CPT Codes for 2024
Let’s go through the CPT codes relevant for dermatology in 2024:
Skin Biopsy
- 11102: Skin tangential biopsy (scoop, shave, curette, saucerize, etc.); individual lesion.
- 11103: Add-on code for skin tangential biopsy, each additional lesion.
- 11104: Punch biopsy of a single lesion and, if necessary, simple skin closure.
- 11105: Add-on code for punch biopsy; each additional lesion.
- 11106: Incisional skin biopsy, such as wedge, including, simple closure; individual lesion.
- 11107: Add-on code for incisional skin biopsy; each additional lesion.
- 40490: Lip excision procedure.
- 69100: External ear excision procedure.
Removal of Lesion
- 17000: Destruction (e.g. laser surgery, electrosurgery, cryosurgery, chemosurgery) of benign or premalignant lesions; first lesion
- 17003: Destruction of premalignant lesions (e.g., actinic keratoses); 2 – 14 lesions
- 17004: Destruction of premalignant lesions (e.g., actinic keratoses); 15 or more lesions
- 17110: Destruction of benign lesions other than skin tags or cutaneous vascular proliferative lesions; up to 14 lesions
- 17111: Destruction of benign lesions other than skin tags or cutaneous vascular proliferative lesions; up to 15 or more lesions
- 11200: Removal of skin tags; up to and including 15 lesions
- 11201: Removal of skin tags; each additional 10 lesions
Mohs Surgery
- 17311: Mohs micrographic technique, including removal of all gross tumor, surgical excision, and repair; first stage, up to 5 tissue blocks on head, neck, hands, feet
- 17312: Each additional stage after the first stage, up to 5 tissue blocks
- 17313: Mohs micrographic technique on trunk, arms, and legs; first stage
- 17314: Mohs micrographic technique on trunk, arms, and legs; each additional stage
- 17315: Each additional block after the first 5 tissue blocks for any location
Pathology
- 88304: Level III – surgical pathology, gross & microscopic exam
- 88305: Level IV – surgical pathology, gross & microscopic exam
- 88312: Special stain including interpretation and report
- 88341: Immunohistochemistry or immunocytochemistry
Laser Therapy and Phototherapy
- 96920 and 96921: Laser treatment for inflammatory skin disease
- 96900: Actinotherapy (UV light)
- 96910: Photochemotherapy; tar and ultraviolet B or petrolatum and ultraviolet B
- 96567: Photodynamic therapy by external application of light to destroy premalignant and/or malignant lesions
- J7308: Aminolevulinic acid HCL for topical administration
Time-based Billing Changes
The evaluation and management billing guidelines for this year have changes related to time. The E/M codes have been revised to remove the time range and instead are based on a single minimum time requirement that must be met or exceeded.
E/M codes and the total time in minutes to meet or exceed:
- 99202 – 15
- 99203 – 30
- 99204 – 45
- 99205 – 60
- 99212 –10
- 99213 –20
- 99214 –30
- 99215 –40
Pathology Update
In pathology, the new CPT codes reference the digitization of glass slides, which aid as add-ons to surgical path codes. The new billing guidelines are:
- 88342 is billed with 0760T
- 88341 is billed with 0761T
- 88344 is billed with 0762T
- 88331 is billed with 0841T
- 88332 is billed with 0842T
- 88302 is billed with 0751T
- 88304 is billed with 0752T
- 88305 is billed with 0753T
- 88307 is billed with 0754T
- 88309 is billed with 0755T
- 88312 is billed with 0756T
Specificity of ICD-10 Codes
In dermatology billing, ICD-10 codes are used to document a variety of skin conditions and their treatments. Each of these codes serves a specific purpose in denoting the medical condition of a patient and can significantly impact the dermatology billing and claim submission. Take cysts, a common condition. In ICD-10, cysts can be coded in many ways – epidermal cyst (L72.0), pilar cyst (L72.11), trichodermal cyst/trichilemmal (proliferating) cyst (L72.12), steatocystoma multiplex (L72.2), sebaceous cyst (solitary steatocyst) (L72.3) and other follicular cysts of the skin and subcutaneous tissue (L72.8). Similarly, eyelid cysts have a separate list of codes – cysts of right upper eyelid (H02.821), cysts of right lower eyelid (H02.822), cysts of left upper eyelid (H02.824) and cysts of left lower eyelid (H02.825).
Introduction of G2211
CMS introduced G2211, a new add-on code for office and other outpatient services that can be listed separately alongside the E/M codes. The CMS code descriptor for G2211 is “Visit complexity inherent to evaluation and management associated with medical care services that serve as the continuing focal point for all needed health care services and/or with medical care services that are part of ongoing care related to a patient’s single, serious condition or a complex condition.”
When billing this code, dermatologists should be aware of the criteria to be met for proper reimbursement. This code will not be reimbursed when billed with modifier 25 on the E/M code for minor procedures. It is to be noted that not all E/M visits are qualified for G2211, as explained in the final rule as “…E/M visit complexity add-on code would not be appropriately reported, such as when the care furnished during the O/O E/M visit is provided by a professional whose relationship with the patient is of a discrete, routine or time-limited nature…”. They provide specific examples of conditions that would not require the add-on complexity code: mole removal, treatment of a simple virus, seasonal allergies, new onset GERD, treatment for a fracture, and/or “when the billing practitioner has not taken responsibility for ongoing medical care for that particular patient with consistency and continuity over time, or does not plan to take responsibility for subsequent, ongoing medical care for that particular patient with consistency and continuity over time.”
As dermatologists need to focus on providing exceptional medical and cosmetic care for patients, keeping track of these changes may be challenging. Working with dermatology medical billing and coding services can ensure practitioners that all the latest updates and criteria regarding dermatology billing are followed accurately. This helps your practice improve patient care by furnishing error-free claims, get appropriate reimbursement, and improve your bottom line.