Claim denials are a silent revenue drain in dental billing, costing practices hundreds of millions of dollars annually. According to the American Dental Association (ADA), around 10% of claims in dental billing face denials with common contributing reasons being coding errors or incomplete documentation. An esteemed advisory board points out that over 90% of these claim denials are preventable.
Effective denial management in dental billing is a strategic process in protecting a dental practice’s financial health, while focusing on patient satisfaction. This post will explore the significance of an efficient denial management in place that can prevent claim denials and streamline this aspect of your dental practice.
What Are the Impacts of Claim Denials in Dental Billing?
- Administrative Constraints: One of the main issues regarding claim denials is the administrative overhead. Handling denials takes up a lot of time involving corrections, reviews and submissions. Usually, the staff handling other responsibilities will have to manage this, leading to increased workload and burnout in practice management.
- Revenue Upheaval: Claim denials result in delayed payment cycles, which can affect a practice’s revenue flow. Unresolved denials over time, will add up and lead to huge losses. Smaller practices that are relying on predictable income for daily operations will have trouble in covering expenses which may jeopardize their permanence.
- Patient Satisfaction: Denied claims usually result in patients shelling money out of their own pockets, giving them a frustrated experience. This dissatisfaction can harm their trust with the practice, negatively affecting retention and referrals. Therefore, addressing billing issues is a must in improving patient experience.
What Are the Most Common Reasons for Dental Claim Denials?
The first step towards resolving claim denials involves understanding the reasons why the claim was denied. Here are some of the common reasons:
- Incomplete Documentation: Insufficient supporting documentation contributes to the majority of claim denials. Certain procedures have mandatory documents to be submitted. Also, all documentation should be legible. It is advised to get in touch with insurers to get clarification on matters which could help prevent claim denials.
- Coding Errors: Using wrong/outdated codes (ICD-10, CDT,) can lead to claims getting denied. The general rule of thumb is to select the code that best matches the treatment required. Also, staying updated with the changes and the types of attachments that each CDT procedure code requires can mitigate the chance of errors.
- Late Submissions: Delayed claim submissions are denied abruptly. Health insurance companies have a deadline for claim filing and it is important to file for claims, right after the dental services are provided. Resubmissions and requests for appeal are usually denied, so make sure to submit the claims before time.
- Duplicate Claims: Repeated submission of a claim may lead to automatic denial of the entire application. Ensure a system is in place to track all claims—applied and in queue and a proper coordination between the staff, to avoid any such discrepancies.
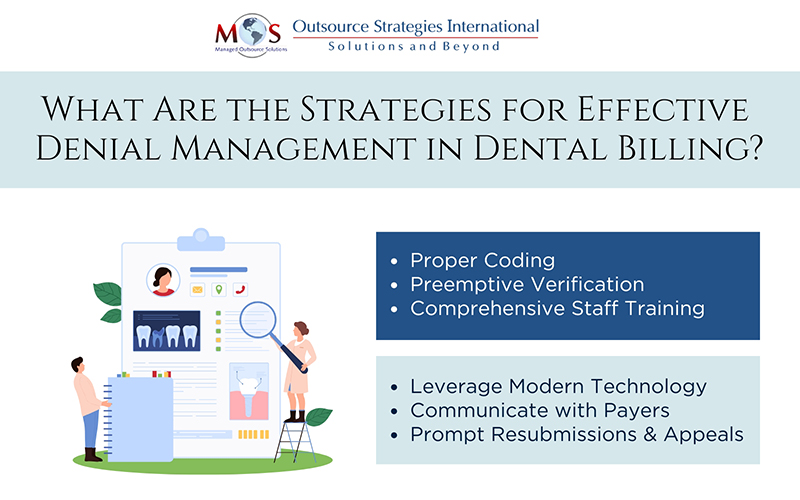
Strategies for Effective Denial Management in Dental Billing
- Accurate Coding & Documentation: Ensure to maintain comprehensive and precise medical records and supporting documentation. Also, using the correct medical/diagnosis codes is necessary for getting the claim sanctioned.
- Advance Insurance Verification: Preemptively verifying patient insurance details, eligibility and coverage plans before starting with the treatment, can help prevent denials by knowing the roadblocks in advance.
- Thorough Staff Training: It is important to educate your staff regarding insurance policies, coding guidelines and best practices to avoid/deal with denials; if that happens. Regular training ensures that the team is prepared adequately for claim submissions.
- Comprehensive Denial Analysis: Once a claim has been denied, it is important to conduct a root cause analysis to find out the reason(s) for denial. This information can then be used for further appeals and/or to be better prepared in the future.
- Leveraging Modern Technology: Investing in state-of-the-art billing and denial management software can automate various time-consuming tasks like claim tracking, identify trends and initiate faster appeals for better results.
- Collaborate with Insurers: Establishing good relationships with payers can help understand their policies/requirements and will help during disputes, in resolving them amicably.
What Are the Benefits of Effective Denial Management?
- Reduced Administrative Hassles: The primary role of a dentist and the staff, would be to focus on their patients and not on billing/claims. A dedicated denial management system will manage everything related to billing, claims and revenue, freeing up the team to take care of critical tasks in hand.
- Improved Patient Experience: A proactive denial management system can mitigate any scenarios involving billing discrepancies and solidify patient trust, which can significantly improve the credibility of the practice and help in retaining patients.
- Better Cash Flow: Efficient denial management can aid practices to track, identify & appeal claim denials, which can help recover lost revenue and thereby, improve the financial health of the practice.
- Optimized Productivity: The filing of claims is one of the major hurdles a dental practice encounters on a daily basis. A proper denial management system can reduce the number of denials and that results in smoother billing workflows and better resource utilization.
Why Partner with an Expert Denial Management Service?
A systematic approach to denial management is crucial to build a positive revenue cycle. However, it requires specialized skills, experience and modern technology to set up a proper denial management system, which most dental practices may lack. An expert dental billing services firm can handle denial management well, owing to their deep industry knowledge, supported by advanced technology, helping them to address root causes and streamline claim submissions and appeals, on time.
Denial management is an inevitable aspect of a successful dental billing strategy. By proactively identifying and resolving root causes of denial, putting into practice efficient processes and enlisting the assistance of an expert, third-party provider like Outsource Strategies International (OSI), can help dental practices optimize their workflow, increase revenue and enhance overall patient satisfaction.
Eliminate Your Dental Billing Hassles with OSI
Collaborate with us & discover how our denial management services can transform your dental practice!