Denial management plays an important role in the complex landscape of healthcare and insurance. Due to its complexity, it also poses a significant challenge. According to a report by the American Hospital Association (AHA), around 15% of all claims submitted to private payers (including pre-approved ones), are initially denied.
This statistic throws light on the significance of having proper denial management strategies in place and promptly addressing denials in medical billing, to ensure financial integrity and operational efficiency of medical practices.
Why Is It Important to Manage Claim Denials?
- Preserving Revenue Flow: Denied claims is one of the reasons why medical practices encounter financial losses. According to the AHA’s report, in 2022, hospitals and healthcare systems spent close to $20 billion in an attempt to overturn denied claims.
- Streamlining Financial Health: High and steady denial rates may drain a practice of its revenue, which in turn, can affect the facility’s capability to make investments in quality patient care, advanced technologies and other resources.
- Ensuring Accuracy & Compliance: When denial management is properly done, it ensures adherence to regulatory guidelines like HIPAA, which subsequently reduces the risk of untimely audits and heavy penalties.
- Sustaining Provider-Payer Relationship: A proper denial management builds a better relationship with payers, expediting a seamless claims process in the future.
Reasons for Claim Denials in Medical Billing
The first step towards managing claim denials involves understanding the common reasons. Here are a few common causes:
- Coding Errors: One of the contributing causes towards claim denials is errors in coding or usage of outdated codes. Now, with the implementation of ICD-11 and other updates, it is important to stay updated.
- Incomplete Documentation: Lack of relevant medical records, inaccurate or missing patient information, or submitting evidence for procedures without proper justification are some of the reasons that can cause claim denials.
- Eligibility Issues: Treatment procedures or services rendered to the patient that were not verified under the insurance policy or authorization are a direct violation and those claims will be denied.
- Late and/or Duplicate Submissions: Claims that were submitted beyond the payer’s deadline will be denied. Also, submitting the same claim multiple times can lead to automatic denial.
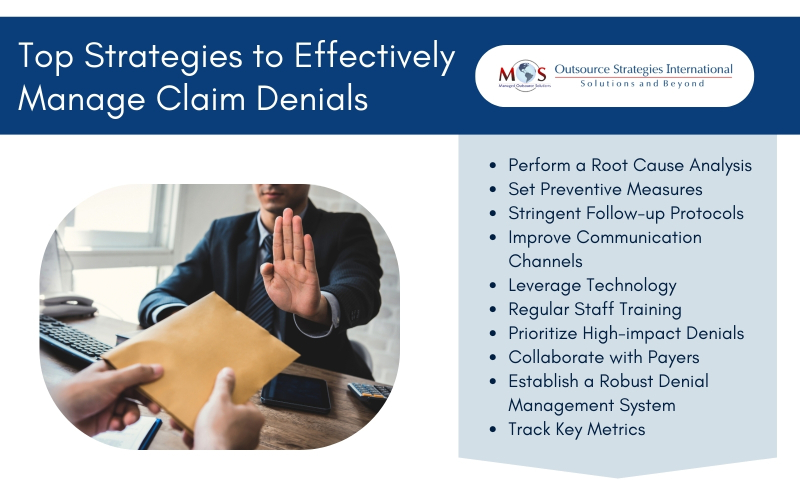
Best Strategies to Handle Claim Denials in a Practice
Implementing robust strategies can significantly reduce denial rates and improve the revenue cycle:
- Perform a Root Cause Analysis: The first step would be to pinpoint the reasons behind denials, which can help address underlying issues more efficiently. This involves analyzing denial patterns to identify errors that happen regularly.
- Set Preventive Measures: After the root cause analysis, preventive measures such as staff training and process improvements can help prevent denials that occur quite often.
- Stringent Follow-up Protocols: Establish strict timelines for following up on denied claims, thereby fostering clear communication with payers which could help resolve issues faster.
- Improve Communication Channels: Foster regular interactions between healthcare providers, admin staff and billing teams, which can help minimize errors and improv
- Leverage Technology: In this fast-paced healthcare system, it has become increasingly difficult to survive without technology. Adopting advanced billing and claims management software can automate processes, reduce errors, and enhance efficiency in handling denials.
- Regular Staff Training: Ensure continuous education on coding updates/changes, regulatory updates, and effective denial resolution techniques to keep staff duly informed and ready.
- Prioritize High-impact Denials: Focus primarily on addressing denials that can significantly affect revenue, thereby ensuring that the resources are allocated effectively for a healthy revenue cycle.
- Collaborate with Payers: Establish engaging relationships with payers to understand their specific requirements. Actively involve in and address any issues that may lead to denials.
- Establish a Robust Denial Management System: The ultimate, recommended solution would be to create a dedicated team or engage a third-party agency to handle tasks such as reviewing, appealing, and rectifying denied claims, ensuring a proactive approach.
- Track Key Metrics: Make sure to regularly track denial rates, causes, and trends to identify areas for improvement and measure the effectiveness of implemented strategies.
Effective denial management is vital for establishing stable financial health and operational efficiency. By identifying the root causes of claim denials and implementing preventive measures, practices can significantly reduce claim denial rates.
Partnering with expert denial management services can help tackle issues regarding claim denials and prevent them from occurring again. Outsource Strategies International (OSI), evaluates each case separately, on its own merits, thereby helping to understand the issue better. We analyze and provide supporting clinical documentation, appeal any prior authorization denials, understand genuine denial cases to pass the responsibility to patients, and follow-up effectively.
Utilizing modern technology, enhancing provider-payer collaboration, and prioritizing staff training are some of the crucial steps involved in this process. A dynamic approach ensures that the denied claims are resolved in a timely manner, the revenue cycle is optimized, and adequate attention is given to patient care. By having proper strategies in place, practices can bypass the complexities of medical billing with confidence and efficiency.
Convert Claim Denials into Approvals
Trust us to handle your claims and maximize your revenue, while you focus on patient care!




