Accurate and ethical medical billing practices play a crucial role in upholding the integrity of the healthcare system. Ethical billing in healthcare not only promotes transparency and trust between healthcare providers and patients but also ensures that healthcare resources are utilized appropriately. In this blog, we explore the significance of ethical practices in healthcare billing and the positive impact they have on patients, healthcare providers, and the overall healthcare process.

Embrace Ethical Billing Standards: Elevate Trust and Integrity
Ethical billing practices are essential for building and maintaining trust between patients and healthcare providers. Patients rely on healthcare professionals to provide them with accurate and clear information about the services they receive and their costs. By ensuring ethical practices in medical finance, healthcare providers showcase their dedication to integrity and transparency, instilling trust in patients and making them feel confident about their healthcare decisions. Providers can ensure ethical billing practices with the support of an experienced medical billing company. They manually review the claims always to ensure that there are no unethical practices such as upcoding or billing for medically unnecessary services. They make sure that the codes assigned are based on the actual documentation provided and not coded higher to maximize reimbursement.


Partner with us for compliant medical billing services that prioritize transparency and accuracy!
Understanding Ethical Practices in Medical Billing
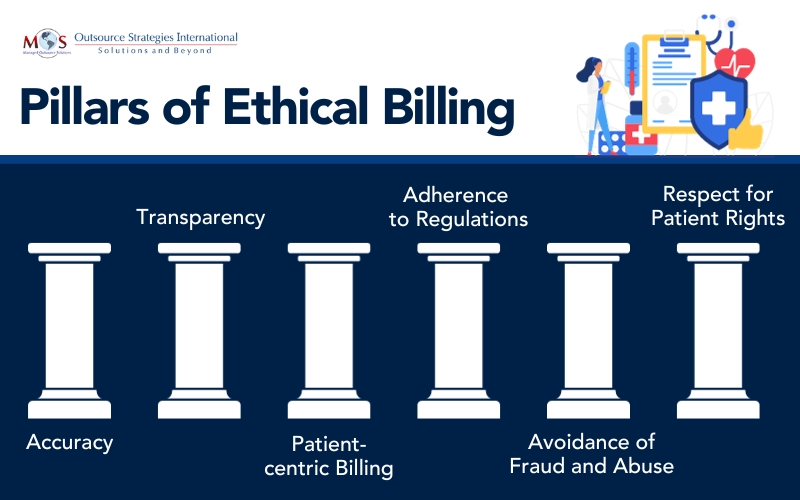
Ethical medical billing means maintaining accuracy and transparency when charging for medical services provided to patients. It ensures that patients are billed fairly, while adhering to ethical standards and professional guidelines. It involves managing billing processes in a way that promotes integrity and honesty, and ensures that patients are charged fairly for the services rendered. The key principles guiding ethical billing in healthcare are:
Transparency
Patients should receive clear and understandable billing statements that represent the services rendered and associated costs. They should be able to easily understand the charges as well as the breakdown of expenses related to their healthcare. For example, after a hospital stay, the patient should be provided with an itemized bill that clearly outlines the charges for each service, procedure, medication, and any additional costs incurred during their treatment. This breakdown ensures transparency, allowing the patient to understand what services they received and the associated costs, promoting trust and accountability in the billing process.
Compliance
Healthcare providers must follow billing laws, including coding standards like CPT codes and insurers’ claim requirements. This involves protecting patient data, adhering to regulations like HIPAA and CMS guidelines. HIPAA compliance ensures secure handling of medical information. Staying updated on regulations is crucial for accurate billing, fraud prevention, and avoiding penalties.
Avoiding Fraud and Abuse
Medical billing fraud is submitting false claims that misrepresent services rendered for greater reimbursement. Adhering to updated ICD and CPT coding standards that accurately reflect the patient’s condition and services provided prevents medical fraud. Avoid fraudulent practices like upcoding, unbundling, misrepresenting services, and duplicate billing. Billing should accurately reflect the services provided and should not involve deliberate manipulation or overcharging.
Respect for Patient Rights
Ethical billing upholds patient rights, ensuring privacy and confidentiality of their information. Bills must detail services and costs in a clear format, supporting patients to comprehend and resolve queries promptly. This includes informing patients about their financial responsibilities and rights to dispute billing discrepancies. By adhering to ethical billing, healthcare providers not only protect patients from financial harm but also contribute to the overall integrity and efficiency of the healthcare system. To succeed, they need to have proper systems in place for maintaining compliance, trust, transparency, and accountability.
Features of an Effective Medical Billing Compliance Program
Ensuring ethical practices in medical finance comes with many challenges. The constantly changing regulations and policies in the complex reimbursement environment pose a specific challenge for professionals striving to uphold ethical standards. Other challenges relate to maintaining confidentiality, health professional-patient communication, professional duty, and decision-making. Developing and implementing a compliance program can overcome these challenges. Based on OIG expertise the components of a robust compliance system include:
- Establishing written policies, procedures, and conduct standards
- Setting up a compliance officer and committee
- Providing comprehensive training and education
- Creating efficient communication channels
- Enforcing standards with clear disciplinary guidelines
- Performing internal monitoring and audits
- Promptly addressing detected offenses and implementing corrective measures

Ethical billing – uphold integrity with compliant medical billing services
Ensure Compliance with the Right Support
Medical billing companies play a crucial role in combating healthcare fraud. In the current healthcare landscape, third-party billing companies have emerged as a vital segment of the industry. Healthcare providers rely on them for processing claims in line with relevant laws, and developing internal controls that ensure compliance with Federal, State, and private health plan regulations. Moreover, these companies assist providers in making informed business decisions. Reliable billing firms collaborate closely with clients to establish and maintain compliance standards for adhering to ethical billing practices.


Struggling with compliance issues? Experience the difference with our ethical medical billing services!