Effective January 1, 2020, all claims submitted to Medicare must be billed with the new Medicare Beneficiary Identifier (MBI) in place of the Health Insurance Claim number (HICN). Starting in 2018, the federal Centers for Medicare and Medicaid Services started sending every Medicare beneficiary a new card designed to better protect against identity theft. Based on the Medicare Access and CHIP Reauthorization Act (MACRA) 2015, CMS was required to remove Social Security Numbers (SSNs) from all Medicare cards. An experienced provider of physician billing services, we are up to date with such updates.
However, there will be limited exceptions for the use of HICNs, such as appeals (People filing appeals can use either the HICN or the MBI for their appeals and related forms), adjustments (HICN can be used for Drug Data Processing, Risk Adjustment Processing, and Encounter Data and retrospective reporting (when submitting data for older contract years for applicable systems).
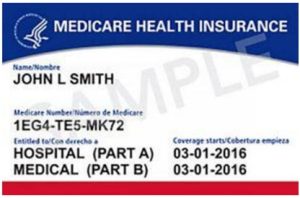
Different from the HICN or SSN and RRB number, Medicare Beneficiary Identifiers (MBI) are made up only of numbers and uppercase letters and are 11-characters in length. No special characters are used and the MBI doesn’t use the letters S, L, O, I, B, and Z to avoid confusion between some letters and numbers.
https://www.forbes.com/sites/nextavenue/2018/03/06/starting-in-april-new-medicare-id-cards/#699e88454192
The beneficiary’s gender and signature have been removed from the newly redesigned cards for additional safeguard against fraud and identity theft.
The new Medicare card entitles a beneficiary to the same Medicare benefits as the old one. MBI will be used in all administrative transactions in which the patient’s insurance coverage must be reported. The MBI will replace the HICN in transactions, including eligibility requests, claims, remittance advices, prior authorization requests, and claim status checks. Practices may not submit both identifiers in the same claim. CMS will respond with the same patient identifier sent by the practice.
CMS recommends using the MBI in the same way as HICN was used. MBI should be placed in the same field of the HICN. Never use hyphens or spaces with the MBI to avoid claim rejections. CMS intends to actively monitor MBI usage during the transition period to verify that providers are prepared to exclusively use MBIs starting January 1, 2020.
How Should Hospitals Prepare for MBIs?
The American Medical Association (AMA) recommends providers to take these steps to adopt MBIs.
Make your systems ready for MBI
Practices should contact their PMS vendors to determine the required changes in their systems to meet those updates. Practices must confirm that their systems can –
- accept and store a beneficiary’s MBI provided by Medicare in the electronic remittance advice for claims submitted with HICNs
- prompt practice staff to ask a patient for the new Medicare card when an eligibility response includes a message indicating that CMS has mailed the beneficiary’s new card
- store both the HICN and MBI, as the practice will need to retain the HICN for other purposes, such as audits, retrospective adjustments, appeals, and collections; and
- identify patients who qualify for Medicare under the RRB and send claims to the RRB Specialty Medicare Administrative Contractor as the MBI, unlike the HICN, will not distinguish RRB patients.
AMA Tips for Practices
To avoid payment delays and workflow disruptions, practices should
- Obtain their Medicare patient’s MBI as soon as possible and store this information in the practice’s PMS
- Educate practice staff about the rollout of the new Medicare cards with the new MBIs
- Make patients aware of the new cards and ask them to bring it with them to their next appointment
- Sign up to MAC’s secure MBI look-up tool. Providers can use this tool to look up patients’ MBIs to bill for things like indirect medical education
- Educate practice staff about the rollout of the new Medicare cards with the new MBIs
- Get the MBI from the remittance advice and save it in systems to use with the next Medicare transaction
To ensure readiness to use MBIs in administrative transactions, hospitals as well as medical billing companies must keep their systems up to date.