Accurate medical billing plays a key role in ensuring any healthcare organization’s financial viability, patient satisfaction, and compliance with regulatory guidelines. It impacts revenue generation, patient-provider relationships, operational efficiency, and overall industry reputation. Proper billing ensures that patients receive correct information about their healthcare costs. It helps them understand their bills, leading to better trust between patients and healthcare providers. Considering the financial health of healthcare providers, billing errors can result in financial losses, and have a negative impact on their ability to provide quality care.
However, medical billing is a challenging process which demands minute attention to details, strict adherence to all applicable rules, and quick processing. It goes beyond simply submitting claims for reimbursement; it encompasses a range of processes and practices that have a significant impact on revenue generation, patient satisfaction, and compliance with regulatory guidelines. Even a single error on a medical claim can lead to claim denial. By utilizing professional medical billing services, leveraging technology, and adhering to regulatory guidelines, healthcare organizations can ensure accurate billing practices, maximize revenue, enhance patient satisfaction, and maintain compliance.
Wondering why accurate billing is crucial?
Let’s discuss in more detail.
Significance of Accurate Medical Billing
The complexities of billing processes, coding guidelines, and ever-changing regulations are the major factors that make accurate medical billing challenging. However, once you successfully navigate these challenges and ensure precision in medical billing, there are many advantages you get to enjoy.


Transform your revenue cycle with our specialized medical billing services.
Call (800) 670-2809 Today!
Reduced Claim Denials
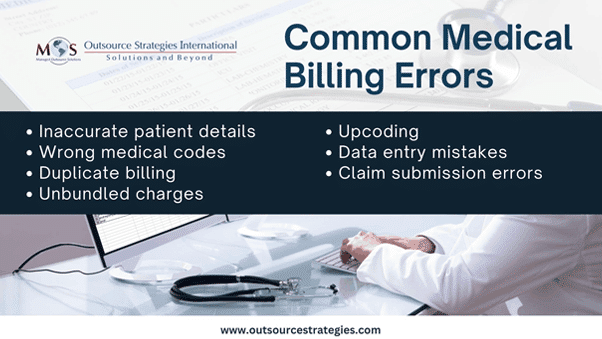
Claim denials are a significant challenge in healthcare revenue management. Inaccurate billing, missing documentation, and non-compliance with payer policies are common reasons for claim denials. Accurate medical billing, supported by thorough documentation and adherence to coding guidelines, minimizes the risk of denials, facilitating a smoother revenue cycle.
According to a survey conducted by Experian Health, the top three reasons for an increase in claims denials are –
- insufficient data analytics (62%)
- lack of automation in claims/denials process (61%)
- lack of thorough training (46%)
When billing information is accurate, it aligns with payer policies and minimizes the risk of errors that could lead to claim rejections. This precision in medical billing not only streamlines the claims process but also enhances the chances of timely reimbursement, ultimately contributing to a more efficient and financially sustainable healthcare operation.
Improved Financial Health
Reducing the likelihood of claim denials leads to a more consistent and predictable revenue stream, preventing financial disruptions that might arise from delayed or denied payments. Accurate billing practices also contribute to efficient revenue cycle management, minimizing the need for extensive resources and time spent on rectifying billing errors or dealing with claim disputes. Additionally, by optimizing the reimbursement process and minimizing revenue leakage, accurate medical billing helps healthcare practices maintain a strong and stable financial foundation, and invest in technology, staff training, and improved patient care initiatives.
Reduced Coding Complexities
Accurate medical billing requires a keen understanding of various coding systems, such as CPT (Current Procedural Terminology), ICD-10 (International Classification of Diseases, 10th Edition), and HCPCS (Healthcare Common Procedure Coding System). The process can streamline coding complexities by ensuring that procedures and diagnoses are precisely documented, eliminating ambiguity. The dynamic nature of healthcare regulations demands continuous education and adaptation to stay compliant.
Patient Care and Experience
Accurate medical billing directly impacts patient care and experience, mainly by preventing financial burdens and delays associated with billing inaccuracies. When billing is precise, patients experience smoother interactions with the healthcare system, reducing stress and promoting trust. Providers can also find more time to deliver high-quality care when they are not burdened by the complications of billing disputes and payment uncertainties.
Compliance with Payer Policies
Different payers have specific policies and requirements for medical billing. Understanding and adhering to these policies are crucial for successful claims processing. It is important for the staff to understand specific coding and documentation guidelines, as well as any changes or updates in policies. Routine internal audits can also identify areas of improvement and ensure that billing practices align with the specific requirements of each payer.

Check out the overview our medical billing process at OSI
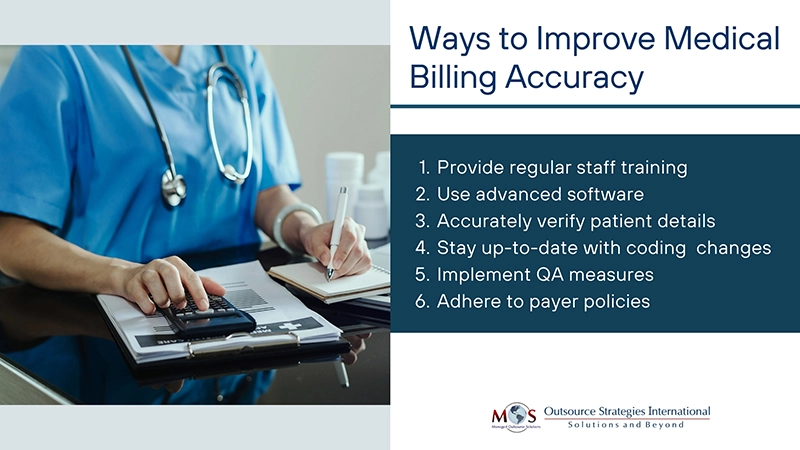
Tips to Improve Accuracy in Medical Billing
1. Conduct regular staff training: Conduct ongoing training sessions for billing staff to ensure they are updated on the latest coding guidelines, regulations, and best practices. This helps them stay informed and reduce the likelihood of errors.
2. Utilize technology: Implement electronic health record (EHR) systems and billing software to automate processes, reduce manual errors, and enhance overall efficiency in medical billing.
3.Double-check patient information: Verify and regularly update patient demographics and insurance details to prevent errors in billing due to outdated or incorrect information.
4. Stay informed about coding changes: Stay up to date on changes in coding systems, such as CPT, ICD-10, and HCPCS, to ensure accurate coding and billing practices.
5. Conduct regular internal audits: Perform routine audits of billing processes to identify and address any discrepancies or areas for improvement. Regular internal checks help catch errors before they become significant issues.
6. Adhere to payer policies: Understand and comply with the policies and requirements of different payers to minimize the risk of claim denials due to non-compliance.
7. Implement quality control measures: Introduce quality control measures to review and validate coding accuracy before claims are submitted, reducing the likelihood of errors.
8. Regularly review and update processes: Periodically review and update billing processes to incorporate industry best practices, address emerging challenges, and maintain a high standard of accuracy in medical billing.
Accurate medical billing is not merely a financial formality but a cornerstone of effective healthcare delivery. Healthcare providers must recognize the importance of precision in billing processes, coding guidelines, and compliance with regulations. By prioritizing accuracy, healthcare organizations can optimize revenue cycles, enhance patient care, and fortify their financial foundations in the ever-evolving landscape of healthcare.