Over the years, there has been a significant evolution in how the healthcare industry handles payment processes. The role played by medical billing software in streamlining and automating diverse financial aspects of healthcare cannot be overstated. This software allows healthcare providers to generate accurate invoices for patient services, monitor payments, handle insurance claims, and ensure adherence to payment regulations. It also simplifies intricate medical billing processes, minimizes errors, and enhances overall efficiency, ultimately resulting in faster reimbursements and improved financial management for healthcare facilities. Providers of medical billing services utilize the latest advanced billing software to ensure accuracy and efficiency.

Medical billing and coding software is designed to effortlessly and precisely manage all intricate procedures and communications associated with revenue cycle management. While software primarily addresses a medical practice’s billing procedures, administrative tasks, and financial processes, Electronic Health Record (EHR) features are predominantly centered on clinical functions, records, and outcomes. Some systems may incorporate clinical EHR functionalities alongside electronic billing and coding to enhance versatility. Let us check out the key benefits of integrating medical billing software for efficiency, providing advantages for both healthcare providers and patients.
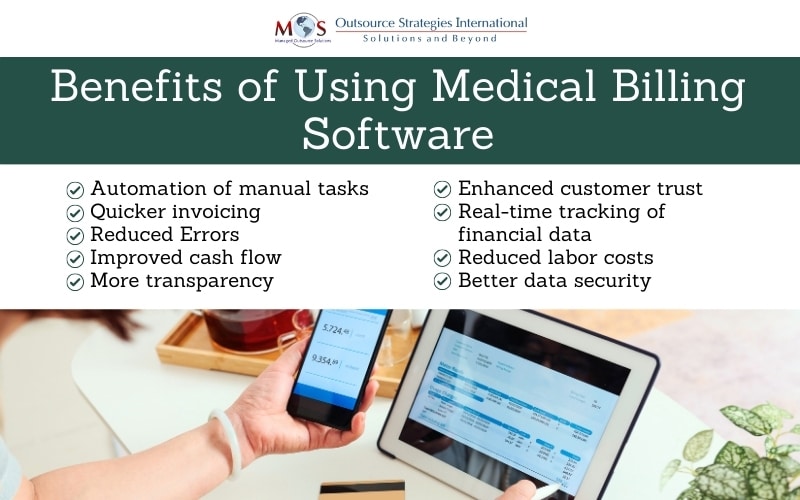
Benefits of Billing Software Integration
Integrating billing software into your workflow can offer other benefits as well, streamlining processes and improving overall efficiency. Here are some key advantages:
- Time savings: A payment processing system automates many manual tasks such as invoice generation, payment processing, and reconciliation, saving significant time and reducing the risk of errors. Automated billing processes result in quicker invoicing, allowing you to send invoices promptly and improve cash flow.
- Accuracy and error reduction: A good billing system eliminates the need for manual calculations, reducing the risk of errors in invoicing and financial reporting. Integration ensures that data is consistent across various systems, minimizing discrepancies and improving overall accuracy.
- Improved cash flow: Automated invoicing and online payment options can lead to faster receipt of payments, positively impacting cash flow.
- Enhanced customer satisfaction: Integration allows for easy and convenient payment options for customers, improving their experience. Automated systems provide detailed and transparent payment information, reducing disputes and enhancing customer trust.
- Financial reporting: Integration enables real-time tracking of financial data, allowing for better decision-making based on up-to-date information. Many billing systems offer customizable reports, providing insights into key financial metrics tailored to your business needs.
- Regulatory compliance: A payment processing system can help ensure compliance with tax regulations and other financial reporting requirements, reducing the risk of non-compliance and associated penalties.
- Cost savings: Automation reduces the need for manual data entry and processing, leading to potential savings in labor costs.
- Data security: Billing software often includes robust security features to protect sensitive financial information, reducing the risk of fraud or data breaches.
By using an advanced invoicing system, healthcare practices can improve their financial processes, reduce manual workload, and ultimately boost their overall operational efficiency.
Tips to Choose the Right Billing Software
Choosing the right billing software is a crucial decision that can impact the efficiency and financial health of the organization. Begin by determining the specific requirements of your healthcare practice. Consider factors such as the volume of transactions, the complexity of RCM, integration needs with other systems, and any specific regulatory compliance requirements.
Other factors to consider include:
- Integration: Ensure that the system can seamlessly integrate with other essential systems in your practice, such as Electronic Health Records (EHR), practice management software, and accounting systems. Integration can streamline workflows and reduce data entry errors.
- Compliance with regulations: Verify that the system complies with relevant healthcare regulations and standards, such as HIPAA (Health Insurance Portability and Accountability Act). Compliance is essential for protecting patient information and avoiding legal issues.
- User-friendly interface: Choose a system with an intuitive and user-friendly interface. This is crucial for the training and adoption of the software by your staff. A user-friendly system can help minimize errors and enhance overall efficiency.
- Automation capabilities: Look for automation features that can simplify billing processes. This includes automated claim submissions, payment posting, and reconciliation. Automation can save time, reduce errors, and improve the speed of revenue cycles.
- Reporting and analytics: Assess the reporting and analytics capabilities of the software. Robust reporting features can provide valuable insights into your practice’s financial performance, helping you make informed decisions and identify areas for improvement.
- Scalability: Consider the scalability of the software. Ensure that it can grow with your practice and accommodate increased transaction volumes and expanding needs without requiring a significant overhaul.
- Training and support: Evaluate the training and support options provided by the software vendor. Adequate training resources and responsive customer support are crucial for a smooth implementation and ongoing use of the billing software.
- Security measures: Prioritize security features to protect sensitive patient data. Encryption, access controls, and regular security updates are essential components of a secure billing software system.
Maximizing software capabilities in medical billing involves a strategic and holistic approach. It’s crucial to thoroughly understand the features and functionalities of the system in use. This includes using automation for routine tasks such as claim submissions, payment postings, and reconciliation to enhance efficiency and reduce errors. Integration with Electronic Health Records (EHR) systems ensures seamless data flow between clinical and billing processes, promoting accuracy and completeness. Regularly updating the software to the latest versions ensures access to new features, improvements, and compliance with evolving healthcare regulations. Additionally, investing in staff training programs ensures that the team is well-versed in utilizing the software’s full potential.
At OSI, we’re up to date with the constantly changing technology in medical billing. Our clients benefit from the latest advancements in the field, enabling them to streamline operations, improve accuracy, and navigate the complexities of medical billing with confidence.