CDT stands for Current Dental Terminology, a standardized set of HIPAA dental procedure codes maintained by the American Dental Association (ADA). Understanding CDT codes and terminology is essential for accurately reporting each dental procedure when submitting claims to dental insurance plans. By using the correct codes, dental practices can ensure that insurance claims are processed smoothly and efficiently, reducing risk of claim denials or delays.

Common Dental Billing Codes
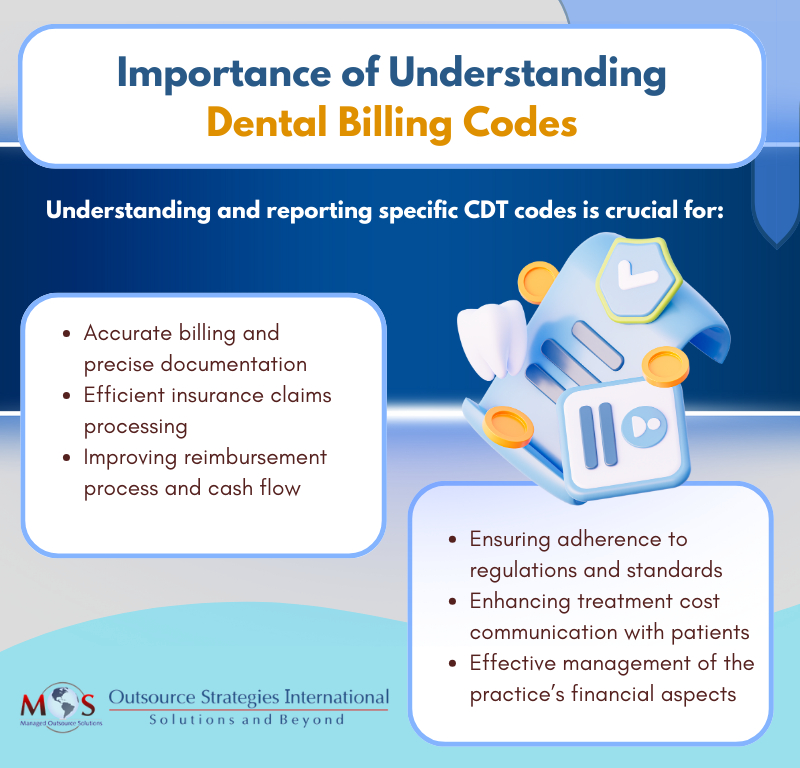
Knowing common dental billing codes is essential for accurate billing, efficient claims processing, appropriate reimbursement, compliance with regulations, and efficient practice management.
Diagnostic Codes (D0100-D0999)
D0120: Periodic oral evaluation – established patient
D0140: Limited oral evaluation – problem focused
D0150: Comprehensive oral evaluation – new or established patient
D0180: Comprehensive periodontal evaluation – new or established patient/
D0210: Intraoral – complete series of radiographic images
D0220: Intraoral – periapical first radiographic image
D0251: Extra-oral posterior dental radiographic image
D0274: Bitewings- four radiographic images
D0330: Panoramic radiographic image
Preventative Codes (D1000-D1999)
D1110: Prophylaxis for adults
D1120: Prophylaxis for children
D1206: Topical application of fluoride varnish
D1351: Sealant – per tooth
Restorative Codes (D2000-D2999)
D2330-D2394: Tooth colored filling – Resin-based composite
D2740: Crown – porcelain/ceramic substrate
D2950: Core buildup, including any pins when required
Stay up-to-date!
The ADA revises and updates CDT codes annually to reflect and accommodate the introduction of new procedures, techniques, and technologies in the field of dentistry, and to facilitate comprehensive patient record-keeping. The annual updates to CDT codes may involve:
- New Codes
- Deleted Codes
- Editorial Revisions
- Nomenclature Edits
- Descriptor Edits

Practices can stay up to date by looking up the resources on the ADA codes website.
Follow Dental Coding Guidelines
By using the right CDT codes on claims to describe the specific procedures and services they provide, dentists can receive appropriate payment from insurance companies, Medicaid, and other payers. To assign CDT codes, the patient must have access to dental insurance. Here are some dental coding basics:
- Dental claims are submitted on the J400 form, which is specifically designed to accommodate dental information. The following dental information must be included on dental claim forms:
- Area of oral cavity
- Tooth system
- Tooth number or letter
- Tooth surface
- Description of procedure
- Missing teeth information
- Use CDT codes to bill dental services. Assign an evaluation CDT code to report an initial, subsequent, or other type of patient encounter.
- When dentists perform medical procedures, they must report them using CPT codes to file claims with medical insurance companies for payment. CPT codes describe the services provided and are reported to the medical carrier on a CMS 1500 claim form. Examples of dental procedures that may require a medical claim form and/or the use of ICD-10 codes include TMJ, maxillofacial surgery procedures, and oral sleep apnea appliance therapy.Here is an example of billing medical insurance and dental insurance for a procedure using CPT and CDT codes.A patient presents to the dentist with symptoms of temporomandibular joint (TMJ) disorder. The dentist evaluates the patient and diagnoses them with TMJ disorder. In this case, the dentist may bill the procedure as both a dental and a medical procedure, depending on the specific services provided.As a dental procedure: The dentist may perform a TMJ evaluation (CDT code: D9310) to assess the patient’s condition. If the dentist administers a treatment such as occlusal adjustment (CDT code: D9951) or fabricates an occlusal orthotic device (CDT code: D9944) to alleviate TMJ symptoms, these procedures can also be billed under dental codes. Narratives and radiograph should be submitted along with the claim.As a medical procedure: If the dentist determines that the patient’s TMJ disorder requires more extensive treatment, such as injections of corticosteroids or Botox for pain management, these services may be billed as medical procedures using the appropriate codes. The appropriate ICD-10 codes should be reported in the correct order. The dentist should also provide documentation to support medical necessity.Medicare instructs that when selecting the procedure or service that accurately identifies the service performed, dentists should use the most accurate code. If CDT code more accurately identifies the service, this should be used rather than the CPT codes.
- Typically, claims with CPT codes are submitted as primary insurance for medical coverage, whereas claims with CDT codes are typically processed as secondary insurance for dental coverage. For correct billing, confirming with the medical insurance provider is to ascertain the primary and secondary payers for a claim.
- The CDT Code and ICD Codes are both HIPAA-mandated standards for electronic dental claims. The American Dental Association states that the ICD diagnosis code set may be used on claims submitted to dental benefit plans when needed, as well as on claims for dental services submitted to medical benefit plans where diagnosis codes are always required. ICD-10 codes in claims filed for dental benefits inform the payer why the procedure was performed and the associated disease, illness, symptom or disorder.
- Dental records should include: Evaluations, Type of Anesthesia, Radiographs, Testing or Diagnostic Service, Documentation of Tooth (Teeth) Treated, and Type of Treatment
It’s crucial to consider the coverage each patient carries. If dental treatment is considered relevant to a medical condition(s), billing medical insurance may be possible, subject to the terms of the insurance policy. This implies patients can seek the same treatment at either their dental or medical office, with different insurance companies billed accordingly. Dental billing experts can help dentists determine whether to submit a medical or dental claim.
Consistent, uniform, and accurate dental code assignment assists dental practices with proper record management and accurate insurance claim submissions. However, navigating the complexities of patients’ dental insurance plans can present a challenging and often frustrating task for dental offices. Fortunately, dental billing services are available to address these challenges. By partnering with an expert dental practices can ensure that insurance claims are processed smoothly and efficiently, reducing the risk of claim denials or delays. This also allows dental practices to focus on providing high-quality care to their patients, while leaving the intricate task of billing and claims management to experts.