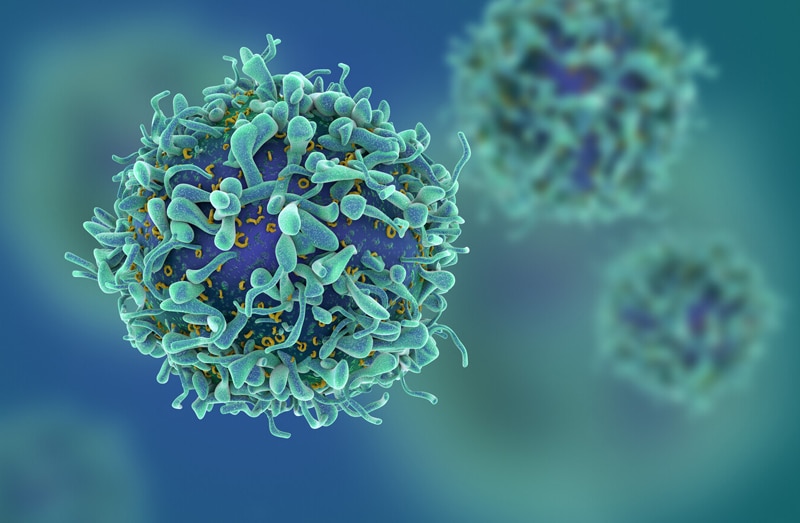
The Centers for Medicare & Medicaid Services (CMS) recently announced its decision to cover the expensive Chimeric Antigen Receptor (CAR) T-cell Therapy for cancers. This cancer treatment uses a patient’s own genetically modified immune cells to fight cancer. The patient’s T cells will be extracted and genetically altered to attack a protein on the surface of the cancer cells and then the cells are infused back into the patient. Experienced medical billing companies train their billing staffs to be up to date with such insurance coverage news.
First of its kind approved by the FDA, there are two CAR-T treatments on the market – Gilead Sciences’ Yescarta for non-Hodgkin lymphoma, and Novartis’ Kymriah for acute lymphoblastic leukemia. The FDA has also approved both treatments for pediatric patients with relapsed or refractory acute lymphoblastic leukemia. Though these therapies are expanding treatment options for certain cancer patients, it still has a big price tag and inevitably comes with CAR T-cell therapy risks.
A Summary on CMS’ Current National Coverage Determination (NCD)
Based on the announcement, CMS will cover the therapy when it is administered at health care facilities enrolled in an FDA-mandated risk evaluation and mitigation strategies (REMS) safety program. The treatment could be given on an outpatient basis, which would be much less costly. The coverage for this therapy will be provided for FDA-approved indications as well as for off-label uses that are recommended by CMS-approved compendia such as ones provided by the National Comprehensive Cancer Network, which are used to determine medically accepted uses of drugs and biologics.
However, the use of non-FDA-approved autologous T-cells expressing at least one CAR is non-covered.
CMS initiated this national coverage determination (NCD) to consider coverage under the Medicare Program for CAR T-cell therapy, for select patients with relapsed or refractory cancers. Treatment protocols for this rapidly emerging adoptive cell transfer immunotherapy vary, but may be summarized in five steps:
- lymphocyte harvesting from the patient with cancer;
- creation of cancer-targeting lymphocytes in vitro using various immune modulators;
- selection of lymphocytes with reactivity to cancer antigens using enzyme-linked immuno-assay;
- depletion of the patient’s remaining lymphocytes using immunosuppressive agents;
- transfusion of the cancer-targeting lymphocytes back into the patient with cancer–this transfusion represents one treatment.
Seema Verma, MPH, CMS administrator said that “As the first type of FDA-approved gene therapy, CAR T-cell therapies are an important scientific advancement in this promising new area of medicine and provide treatment options for some patients who had nowhere else to turn.”
The recent announcement makes it clear that CMS will be paying not only for CAR T but all the related services – the administration of the drug, the collection of the cells, the manipulation of the cells and then putting it back into the patient. And, any of their outpatient or inpatient care as well.
Coding guidelines
CMS has recommended that for claims submitted on or after April 1, 2019, it is required to submit CAR T-cell-related revenue codes 087X (Cell/Gene Therapy) and 089X (Pharmacy) established by the National Uniform Billing Committee (NUBC). When billing charges separately for tracking these services when furnished in the outpatient setting, providers must submit:
- HCPCS 0537T with revenue code 0871
- HCPCS 0538T with revenue code 0872
- HCPCS 0539T with revenue code 0873
Remember that Medicare pays for the administration of CAR T-cells in the hospital outpatient setting separately under CPT code 0540T with Revenue Code 0874, which is assigned to status indicator “S”. For Medicare payment, it is recommended to include the charges for all the steps involved in the charge submitted for the biological or report these charges separately for tracking purposes.
In February 2019, a proposal was made for “coverage with evidence development” – which would have required hospitals to collect and report data on patient outcomes over a long period. However, CMS’ final decision dropped that data collection requirement. Instead, it was decided that the agency will rely on patient information collected by the Food and Drug Administration (FDA) and the National Cancer Institute.
Though the agency has planned to make a coverage decision in May, it was delayed as there was uncertainty regarding figuring out how to cover and pay for the treatment. The reluctance was related to the excessive costs associated with CAR T-cell therapy, which run around $375,000 to $475,000, depending on whether it is used for patients with advanced lymphoma or pediatric leukemia. And if these patients end up requiring hospitalization, which is variable, it can cost hundreds of thousands of dollars more. Along with its sister agencies, CMS will monitor outcomes for Medicare patients receiving this innovative therapy going forward. While choosing a medical billing and coding company, oncologists must make sure that the firm is aware of the changing insurance coverage and billing and coding requirements as well.