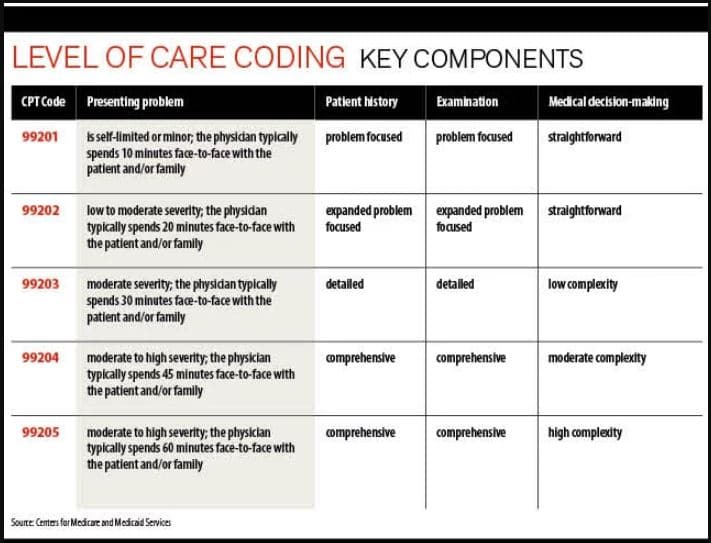
The evaluation and management (E/M) patient visit is the most common element in family practice medical billing. Billing the correct E/M level is necessary to avoid loss of revenue, payer billing and coding audits, and payment recoupments. Often, practitioners choose an E/M level that is too high or too low. There are several reasons for this: lack of understanding on using the E/M codes, complex documentation requirements, and the subjective nature of the medical decision making (MDM)element. The Centers for Medicare & Medicaid Services (CMS) introduced significant changes to the coding and documentation of office visit E/M services (codes 99201-99215) in 2019. Physicians need to meet E/M documentation requirements so that medical billing and coding companies can help them bill the correct level of care.
The basic components of E/M codes are:
-
- Chief complaint (CC)– Purpose for the patient encounter, typically the chief complaint in the patient’s own words
- History of Present Illness (HPI)– Description of the CC
- Location
- Duration
- Severity
- Context
- Quality
- Timing
- Modifying factors
- Associated signs and symptoms
- Review of Symptoms (ROS) – The patient is asked questions for recognizing symptoms the patient currently has or has had in body systems.
- Past, Family, Social History (PFSH)
- Examination – The levels of E/M services are based on four types of examinations:
- Problem Focused – Limited examination of the affected body area or organ system
- Expanded Problem Focused – Limited examination of the affected body area or organ system and any other symptomatic or related body area(s) or organ system(s)
- Detailed – Extended examination of the affected body area(s) or organ system(s) and any other symptomatic or related body area(s) or organ system(s)
- Comprehensive – General multi-system examination or complete examination of a single organ system
- Medical Decision Making (MDM) -MDM refers to the complexity of establishing a diagnosis and/or determining a management option. There are four levels of MDM: Straightforward; Low complexity; Moderate complexity, and High complexity. Selection of the level is based upon the number of diagnoses, amount of data analyzed, and risk of complications.
Source: Medical Economics, November 25, 2014
According to a recent Medical Economics article, to increase revenue and reduce audit risk, physicians need code accurately to represent the specific elements for each E/M level. Care must be taken to avoid down coding and up coding.
Up coding is reporting a higher-level service or procedure or a more complex diagnosis, than is supported by medical necessity, medical facts, or the provider’s documentation. Physicians should also avoid reporting the same E/M level for all patients with the same diagnoses (e.g., diabetes or congestive heart failure), without taking medical necessity into account.
Under coding or down coding occurs when the physician fails to provide relevant documentation details to assign a service, procedure, or diagnosis to the optimal level of specificity. In addition to potentially harming the patient, under coding leaves revenue on the table as the service billed reimburses less than the service actually performed.
In 2019, physicians have a new time reporting option. They can select a code based on the total length of the visit even if counseling did not dominate the service time. The new rules eliminated the previous requirement that greater than 50 percent of the visit must be spent in counseling or coordination of care. Typical times (in minutes) for new and established office or other outpatient E/M services are as follows:
| New patient visits and typical time (in minutes) | Established patient visits and typical time (in minutes) |
| 99201 – 10 | 99211 – 5 |
| 99202 – 20 | 99212 – 10 |
| 99203 – 30 | 99213 – 15 |
| 99204 – 45 | 99214 – 25 |
| 99205 – 60 | 99215 – 40 |
Medical Economics offers the following documentation tips to ensure billing and coding of E/M services:
- For Level 4 or 5 patient E/M codes 99204 or 99205,documentation must include one specific item from the past medical history, one specific item from the family history, and one item from the social history
- To prevent down coding, document a review of systems that relates directly to the problem identified in the history of the present illness (HPI) as well as a review of all additional body systems
- For level 3 patient E/M code 99203, document one specific item from either the past, family, and/or social history that is directly related to the problem in the HPI
- For HPI, documentation should specify the location, quality, severity, timing, context, modifying factors, and describe associated signs and symptoms significantly associated with the presenting problem.
- To avoid repetitive HPI and cloning documentation, providers should document any new symptoms that the patient has or provide evidence that the patient has been stable and symptoms are controlled.
- Review only body areas or organ systems that affect MDM for the current encounter. For e.g., the patient would not require a multi-system exam in subsequent visits. Pulling in this information from the initial visit can amplify the E/M level and increase audit risk.
- If levels 4 and 5 are reported with negative findings, the physician should explain the analysis in the context of the patient’s complaints.
- Physicians can report encounters based on 1995 or 1997 E/M guidelines. The 97 guidelines allow additional options for single organ system exams, so that providers can report higher-level services for intensive, problem-specific examinations. Physicians should verify with their local Medicare Administrative Contractor (MAC) and other payers to determine the amount and complexity of the exam components required. The relevant guidelines should be integrated in the practice EHR system.
- Knowing how payers calculate MDM and documenting all the necessary elements can support higher-level E/M code assignment.
- The documentation must include the total time in minutes that was spent face-to-face with the patient and/or family during the visit, along with how much time (in minutes) was spent counseling the patient and/or family or coordinating care. It is also important to summarize what was discussed with patient and/or family.
- Avoid underpayments by taking care not to report a lower-than-necessary E/M level or not documenting all of the services rendered or the complexity of the MDM.
Partnering with an experienced medical billing company is the best way to ensure proper reporting of E/M services. Reliable companies will help practices conduct periodic, internal audits of their coding, billing, and documentation practices to detect and eliminate up coding, down coding and other compliance risks.




