In the complex world of medical billing and coding, modifiers serve as powerful tools that can significantly impact reimbursement and claims processing. Sometimes a CPT or HCPCS code is not enough to tell the story of a patient encounter. Modifiers are used in such situations to provide additional information about the medical procedure, service, or supply represented by a CPT code, without changing the meaning of the code. Leveraging expert medical billing services can help physicians use modifiers correctly and better inform payers what services took place and also how those services should be reimbursed.

Not using modifiers correctly can lead to claim denials, delays and audits
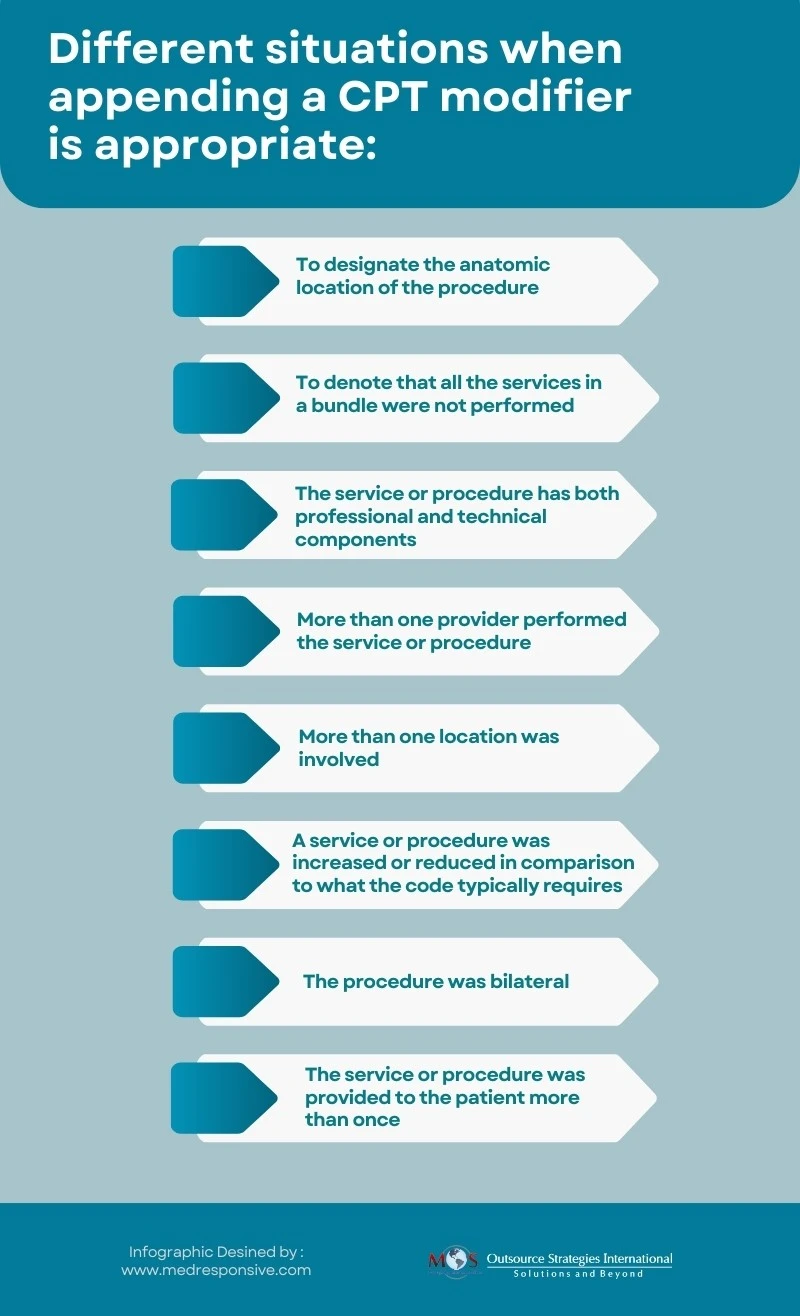
Let’s look into the significance of modifiers, their usage, and crucial role in accurately reflecting the complexity of medical procedures and services.
What is a Modifier in Medical Billing?

A modifier serves as the “means to report or indicate that a service or procedure that has been performed has been altered by some specific circumstance but not changed in its definition or code.”
A medical coding modifier consists of two characters (letters or numbers). When added to a CPT code or HCPCS code, a modifier provides additional information necessary for processing a claim, such as how, where or why the procedure was performed.
The American Medical Association (AMA) updates CPT codes and modifiers annually.
Guide to Modifier Codes in Healthcare
Common Modifier Codes in Medical Billing
CPT modifiers are added to the end of a CPT code with a hyphen. Here are some different types of CPT modifiers used in medical billing:
- 25: Significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of the procedure or other service
- 26: Professional component
- 52: Reduced services
- 53: Discontinued procedure
- 55: Postoperative management only
- 56: Preoperative management only
- 59: Distinct procedural service
Example of Modifier 25 in Action
A patient visits a physician’s office for a regular check-up and, during the same visit, the physician also performs a minor procedure, like removing a small skin lesion.
In this scenario, if the physician appends Modifier 25 to the CPT code when submitting the claim, it signifies that a significant, separately identifiable service was performed during the same visit as the check-up.
When modifier 25 is added to the CPT code, it helps distinguish the additional procedure from the routine check-up, allowing the physician to receive reimbursement for both services.
Without Modifier 25, the insurance might view the procedure as part of the routine check-up and could potentially deny separate reimbursement for the procedure.
HCPCS Modifiers
HCPCS Level II modifiers are alphanumeric, with a letter being the first character of the code. Like CPT modifiers, they provide additional information about a procedure or service without redefining the service provided.
For example:
AA: Anesthesia services performed personally by the anesthesiologist.
AD: Medical supervision by a physician: more than four concurrent anesthesia procedures.
Using Modifier Codes for Accurate Billing – Key Points
Modifiers tell the story of a procedure and can impact payments. Here are some key points on modifier use for medical billing:
Modifiers are classified as pricing (affecting payment) and informational. Medicare prioritizes reimbursement modifiers before informational ones on claim forms.
Using a modifier doesn’t guarantee reimbursement; payers might request documentation to support the use of the assigned modifier.
Insurance or third-party payer rules on modifier use vary with specific HCPCS and CPT billing codes. Not all modifiers can be used with HCPCS or CPT codes.
Incorrect use or absence of modifiers can lead to claim rejection or audits, especially with government programs like Medicare and Medicaid. Moreover, some HCPCS and CPT modifiers are mutually exclusive; for instance, Modifier 50 denotes a bilateral procedure, while Modifiers LT and -RT specify body sides.
Understanding these modifiers is pivotal to navigate the intricate landscape of billing and coding, ensuring proper documentation and reimbursement for services rendered. Expert medical billing and coding services can ensure accurate coding and proper modifier usage in compliance with payer regulations, facilitating quick and accurate reimbursements.