Patient scheduling is one of the most critical administrative tasks that have to be implemented efficiently in healthcare settings. It involves several tasks, such as booking appointments, sending reminders, and managing cancellations. Systematic front-desk management is pivotal to handling patient flow, rendering quality care, and enhancing overall service experience.
Although the medical appointment management process may seem straightforward, it involves various complexities and nuances that healthcare providers must navigate. A disorganized clinical appointment process has severe consequences, including increased no-shows, financial strain, and reputational damages for practices. To mitigate these risks, health facilities can opt to outsource to a medical billing company to handle their scheduling process and focus on healthcare activities.
Partner with our medical billing services to streamline your RCM process, reduce errors, and increase revenue!
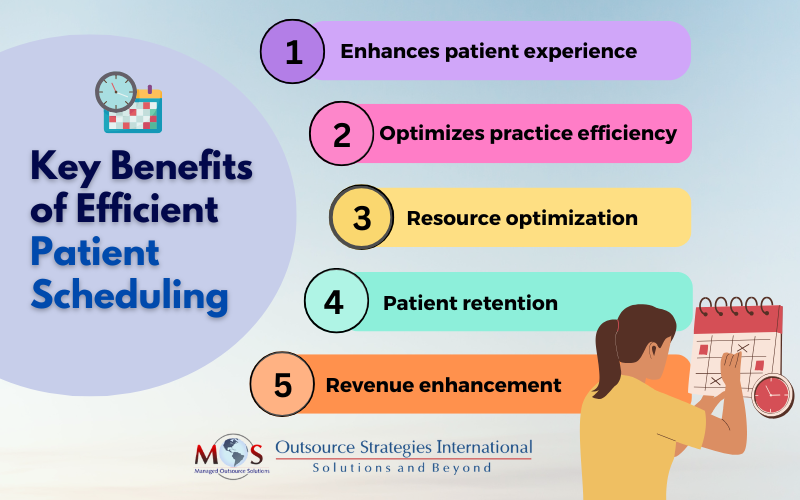
Key Advantages of Patient Scheduling
Healthcare providers can unlock the following benefits by implementing best practices for medical appointments:
- Enhance patient experience: Patients appreciate minimal wait time, and optimizing scheduling processes leads to better quality care, boosts health outcomes, and enhances overall patient satisfaction. By strengthening healthcare provider-patient communication and interaction with scheduling systems, practices can foster trust and build long-term loyalty.
- Optimize practice efficiency: A streamlined scheduling process enables a systematic and structured operational workflow in medical facilities. Delays in patient care may lead to inefficiencies such as administrative burdens, unexpected expenses, and employee turnover. By fostering a culture of efficiency, practices can improve staff competency, better allocate resources, and maximize revenue.
- Resource optimization: Efficient scheduling enables better resource planning, allocation, and use to maximize productivity. It noticeably reduces time spent on manual tasks to optimize operational workflow and minimize obstacles of healthcare organizations. Maximizing the functionality of resources such as staff, equipment, and instruments leads to improved efficacy and performance of the practice.
- Patient retention: Automated patient appointment booking system for clinics and hospitals through online self-booking, automatic reminders, and smart waitlists makes it easier for patients to receive the care they need. By reducing wait times with a stable and predictable schedule, practices can minimize no-shows and last-minute cancellations. A seamless patient journey therefore translates to better clinical condition, improved patient safety practices, and overall enhanced patient retention.
- Revenue enhancement: Affordable doctor appointment scheduling solutions can help practices optimize provider productivity and appointment slots, ultimately maximizing revenue for the services provided. A proactive approach to patient communication with timely confirmations and reminders ensures minimal cancellations, leading to efficient resource usage and better financial strength for practices.
Best Practices to Optimize Appointment Scheduling
Clinical administrators can follow the given set of best practices by aligning practice capability and infrastructure with clinical visit rate to maximize revenue flow:
- Implement a self-schedule system: Health facilities can implement a self-scheduling patient booking system that allows patients to book appointments at their own pace and convenience. Websites can have user-friendly features such as real-time availability, latest updates, and automated reminders. With this arrangement, practices can reduce staff workload, offer flexibility, and improve patient access.
- Prioritize appointments: Consider factors such as medical urgency, time requirement, and geographical proximity while booking appointments. Medical professionals should use their best judgment for a patient’s condition and prioritize according to medical emergencies. Utilize robust technologies such as AI and predictive analysis to predict patient’s volume, determine daily peak time, and decide the appropriate level of time for care.
- Create a waitlist: Leverage smart clinic scheduling tools to create digital waitlists that send out automatic messages to patients for updating their appointment status. This provides an opportunity to fill in any booking gaps and keep your schedule full in case patients cancel their appointments last-minute. Digital waitlists can help retain patients as they do not have to constantly inquire about their current status and also receive slots for earlier appointments.
- Use automated reminders: The key to maintaining consistent scheduling is minimizing the amount of cancellations, no-shows, and missed appointments that occur in a day. Use automation to maintain clear communication with patients by sending customized reminders via texts, emails, or phone calls. Since underutilized appointment time causes disruptions such as overhead costs, wasted resources, and lost revenue, automated appointment reminders allow you to anticipate demand and allocate resources efficiently.
- Implement appointment policies: Consider implementing strict clinical scheduling policies for your practice to reduce no-shows, avoid overbooking, and ensure regular patient throughput. Adopt rules for appointments by charging a fee after a specific timeframe for late or missed visits. Unlike other services that may benefit from a first-come, first-served basis, medical entities need to adhere to an organized schedule to manage their service delivery.
- Embrace an automated recall program: Establish customized patient outreach, recall, and follow-up routines by sending automatic, personalized reminders. It contributes to continuity of care and eliminates scheduling conflicts such as overlapping appointments, reducing the likelihood of no-shows. This type of system boosts the timely flow of patients, ensuring that the practice doesn’t face a dearth or overflow of services.
- Track schedule performance: Monitor key metrics such as wait times, no-shows, and satisfaction scores to gauge the performance of your clinical scheduling process. Frequent analysis will help practices to find bottlenecks, adversaries, and areas of improvement. Identify and follow industry trends to fine-tune the scheduling process for greater efficiency.
Managing patient appointments in-house involves a host of operational and financial challenges, which practices can address by investing in reliable healthcare scheduling services. These outsourcing companies automate appointment booking process, providing a multitude of benefits and reducing errors for healthcare institutions. By integrating modern scheduling tools with billing systems and adhering to best practices in medical scheduling, they streamline the processes to boost efficiency and minimize revenue cycle delays. This proactive approach not only alleviates administrative burdens but also improves the patient experience and drives revenue growth.




