For any kind of practice, an efficient medical billing process is essential to ensure smooth submission and follow up on medical claims. When it comes to receiving timely payments, accurate billing and coding are key. Accuracy also ensures that patients are billed correctly and fairly. A growing number of practices now rely on medical billing outsourcing to ease the cumbersome billing process, avoiding claim denials and maximizing reimbursement.
Before getting into detail on how outsourcing can maximize reimbursement, let’s consider the nature of reimbursements. Private insurers and government agencies such as Medicare and Medicaid are major factors. They each have individual rules, regulations, guidelines and reimbursement rates, all of which add to the complexity of the entire process. Also, the reimbursement amount may vary based on the diagnosis, treatment provided and where it was provided, among other factors. When preparing the medical claim, you must have a clear understanding of all these details to ensure maximum reimbursement.
Partnering with a knowledgeable billing company can help physicians minimize denials and get paid on time and for the maximum amount. Reliable companies successfully handle the entire revenue cycle management (RCM) process – from patient scheduling, insurance verification and medical coding, to accounts receivable (AR) management and financial reporting.


Ready to reduce administrative burden and improve cash flow?
Schedule a consultation to explore the benefits of medical billing outsourcing!
Call (800) 670-2809!
Maximizing Reimbursement by Outsourcing Medical Billing
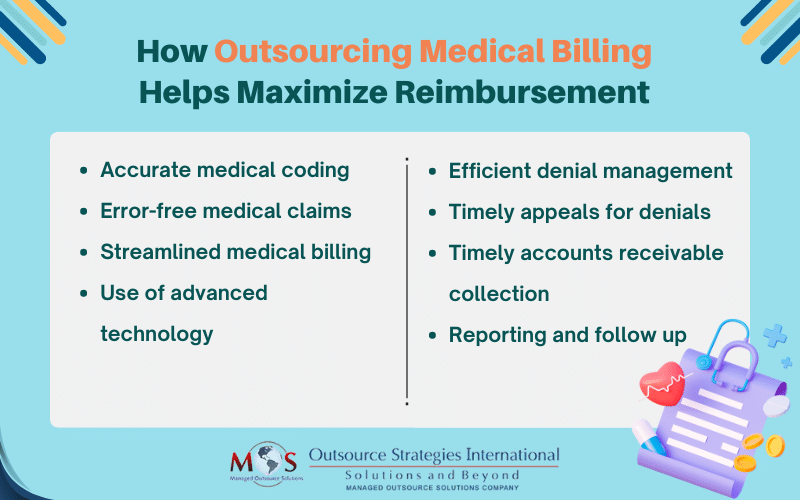
Here’s how can you maximize reimbursement by outsourcing your medical billing process:
- Accurate assignment of medical codes: Accurate coding is at the core of optimizing reimbursements. The right codes enable healthcare providers to unambiguously describe the medical services provided. This in turn ensures appropriate reimbursement. Medical billing companies have trained and experienced medical coders with expertise in medical coding and billing practices. They are regularly trained and educated in coding and billing so that they can ensure compliance with the latest coding guidelines and maximize reimbursement. Professional coders and billers stay up to date with HIPAA, Medicare and other regulatory requirements. Additionally, they perform audits on a regular basis to identify any compliance issues and promptly adopt corrective measures.
- Ensures the claims are error-free: Experienced medical billers avoid common errors such as erroneous patient information, incorrect medical codes, missing or incomplete details, duplicate billing, billing for non-covered services, coordination of benefits errors, and untimely filing.
- Streamlined medical billing: Dedicated staff take care of all vital processes starting with the submission of claims and following up on them, to denial management. With minimal billing errors and quick turnaround times, you get paid quicker and more accurately.
- Use of advanced technology: When it comes to optimizing revenue cycle management, you need state-of-the-art billing and reporting systems. Outsourcing companies utilize advanced billing software and technology platforms that are customized to the specific needs of your practice. These help spot coding errors, keep track of claims status, and increase billing efficiency. You will also get comprehensive reports analyzing your practice performance. This will ultimately help enhance reimbursement and overall revenue.
- Efficient denial management: Claim denials and loss of revenue are major concerns for medical practices. When outsourcing, providers will benefit from the proactive denial management strategies followed by the partnering company. They conduct a thorough study of denial trends – from the information gathered, they develop and implement corrective actions and appeal denied claims in a timely manner. This is a sure way of maximizing provider reimbursement.
- Improved patient satisfaction and smoother financial transactions: Billing errors will not only affect your practice revenue, it can also frustrate patients. A survey from Zelis and Hanover Research highlights that patients are frustrated with the healthcare billing process, and they struggle with identifying and solving billing errors. This survey that gathered answers from 800 US consumers shows that:
- 41% consumers reported being significantly frustrated with addressing errors.
- 50% of the respondents reported incorrect charges of at least $200, while a quarter reported billing errors of $500 or more.
With dedicated billing professionals managing claims submission, follow-ups, and payment processing, patients experience fewer billing-related issues and delays, leading to smoother financial interactions.
Medical Billing Outsourcing Is a Practical Solution
Based on the above points, it’s clear that the best way for providers to optimize their reimbursements is to utilize innovative outsourcing solutions. This will enable them to significantly enhance RCM efficiency. The cutting-edge technology that’s used is designed to improve coding and documentation efficiency and optimize the entire billing process.
At OSI, we take pride in our analytic and reporting capabilities that give providers a clear view of their RCM performance. These insights also help identify any areas that need improvement, and once identified, effective strategies can be implemented to enhance revenue.
Robust documentation practices, coding training, regular audits, and streamlined RCM strategies are vital for increasing revenue in any practice. Great billing companies can also help with coding complexity questions and issues, regulatory compliance and payer denials. These companies can also free up time spent on tedious administrative tasks to focus on patient care and other core tasks. Outsourcing provides access to advanced technology and analytics tools, enabling practices to gain valuable insights into their financial performance and make informed decisions for growth.
Success when outsourcing depends on careful selection of a reliable partner, establishing effective communication channels, and maintaining proactive oversight and quality control measures. A medical billing company with years of experience in the field is well-positioned to provide cost-effective solutions for individual physician offices, family practices, clinics, hospitals, and any other specialty practice.