Just like in any other specialty, accurate billing is crucial in dental practices too. It is essential to running a dental practice because it affects the practice’s financial stability and profitability. Dental billing has become a complex and critical task as the importance of dental care has grown. Accurate dental billing ensures financial steadiness by securing correct reimbursement for services rendered, and covering operational expenses. It also enhances patient satisfaction, as it reduces confusion regarding billing matters, thus raising trust and loyalty. Efficient revenue cycle management is another benefit, as it helps restructure payment processing, reduces delays, and improves reimbursement rates. By maximizing revenue through proper coding and documentation, dental practices can strategically enhance their financial performance.
Outsourcing the task to a professional dental billing company can simplify administrative processes and free up valuable time for dental practices to focus on patient care. Combining expertise and technology, outsourcing can also improve billing accuracy, reduce claim denials, and maximize revenue potential for the practice.
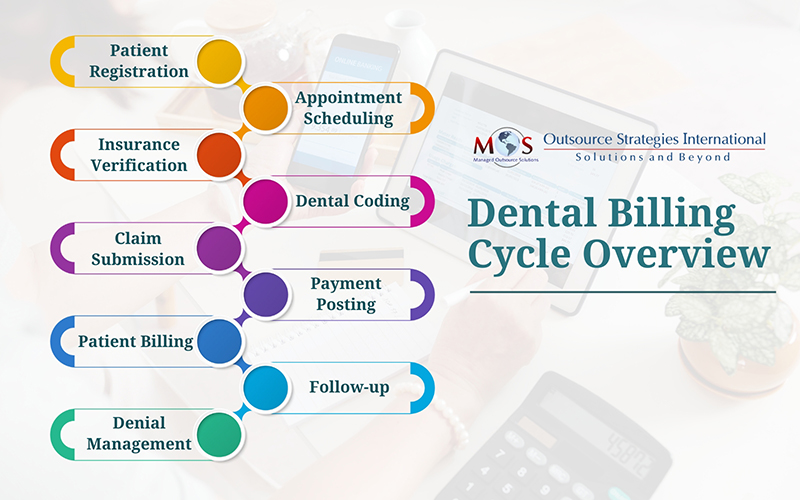
Let us check out the dental claims processing steps here.


Ready to boost your practice’s bottom line?
Let our dedicated team handle your dental billing needs with precision and efficiency.
Dental Billing Process Explained
The dental billing process involves the submission and processing of claims for dental services provided to patients. Here’s an overview of the steps involved:
- Patient registration: The dental billing process starts with patient registration, where patients’ personal and insurance information is collected and entered into the dental office’s database. During this crucial stage, dental offices collect comprehensive patient information, including personal details and insurance coverage. Thorough registration ensures that the billing staff can accurately verify insurance benefits, eligibility, and any pre-authorizations required for planned procedures. It also simplifies communication with insurers and minimizes delays in claim processing.
- Patient appointment scheduling: Dental offices must carefully coordinate appointments to ensure that providers’ schedules align with patient needs and preferences. Accurate scheduling also plays a key role in maximizing productivity along with reducing wait times for patients. By maintaining organized appointment calendars and using efficient scheduling software, practices can improve operations, increase patient satisfaction, and thus achieve a smoother billing process.
- Insurance verification: Dental insurance verification plays a key role in ensuring seamless and accurate processing of claims. Billing specialists verify the patient’s insurance coverage, including benefits, eligibility, and any pre-authorizations required for specific procedures. By thoroughly understanding patients’ insurance plans, practices can avoid misunderstandings, ensure proper billing, and prevent unexpected costs for patients. Proper verification also reduces claim denials, and improves overall efficiency in managing patient accounts.
- Coding: Each dental procedure performed is assigned a specific code from the Current Dental Terminology (CDT) code set, for billing purposes. The codes describe the procedures in a standardized way, making it easier for insurance companies to process claims. CDT codes accurately describe the specific dental treatments, services, and procedures provided by dental practitioners. Proper coding also ensures that insurance companies understand the nature and complexity of the services rendered, facilitating accurate reimbursement for both patients and dental practices.
- Claim submission: Once the treatment is completed, the dental office or the billing company submits a claim to the patient’s insurance company. The claim includes details such as the patient’s information, provider information, service codes, and fees. Accuracy and completeness are crucial during this stage to avoid delays or denials. The insurance company reviews the claim, assessing factors such as the patient’s coverage, the provider’s participation in the network, and the medical necessity of the procedures performed. Once approved, the insurance company disburses payment to the dental office, covering the agreed-upon portion of the treatment costs.
- Payment posting: After claims have undergone adjudication and insurance companies have processed them, payment posting involves reconciling the amounts received with the expected reimbursements outlined in the Explanation of Benefits (EOB). This process requires attention to detail to ensure that payments are correctly allocated to specific services provided, taking into account any co-pays, deductibles, or adjustments. The process involves updating the patient’s account balance, reflecting the remaining amount owed or any credits that may apply.
- Patient billing: Patient billing involves generating and sending invoices or statements detailing the services provided, the insurance payments received, and the patient’s responsibility. Clear and transparent communication regarding financial obligations is essential to ensure patients understand their bills and can make timely payments. Dental practices may offer various payment options, including online portals, installment plans, or assistance programs for those facing financial hardship.
- Follow-up and denial management: In some cases, claims may be denied or require additional information. The dental office follows up with the insurance company to resolve any issues and ensure timely payment. Regular follow up is important to know about the status of pending claims, identify reasons for denials or rejections, and provide any additional information or documentation required for claim adjudication. Denial management addresses claims that have been rejected or denied by the insurer. The dental billing staff reviews denial reasons, identifies patterns or trends, and takes corrective actions to appeal denials, resubmit claims with necessary corrections, or pursue alternative avenues for reimbursement.
Overall, when utilizing dental billing services, it requires proper coordination between dental staff, patients, and insurance companies to ensure accurate and timely payment for services rendered.
When selecting a dental billing company, it’s crucial to consider several key factors such as – the company’s expertise and experience in dental billing, track record of success, knowledge of industry-specific regulations and coding guidelines, technology infrastructure and billing software capabilities, as well as their commitment to staying updated with the latest advancements in billing technology.


Transform your dental billing experience with our tailored solutions!
Partner with us today.