Failure to obtain proper prior authorization is one of the key reasons for claim denials in many medical specialties, and radiology is no exception. Radiology prior authorization is meant to ensure that physicians follow proven guidelines when ordering imaging tests. This helps protect patients, improve the quality of care, and make sure imaging tests are used correctly and safely. Whether you are an imaging specialist or a referring physician, submitting prior authorizations to insurers ensures that the service prescribed by a patient’s physician is covered by their health insurance plan. Radiology prior authorization services ease this cumbersome and time-consuming administrative process, allowing patients to undergo the procedures they need in a timely manner.


Simplify your radiology approvals with our insurance verification and prior authorization services!
Radiology Procedures that need Prior Authorizations and Their CPT/HCPCS Codes
Radiology exams that may require pre-authorization include:
- Bone Mineral Density exams ordered more frequently than every 23 months
- CT scans (all diagnostic examinations)
- MRI/MRA (all examinations)
- Nuclear medicine studies including nuclear cardiology
- PET scans
- Stress echo cardiograms
Insurers do not typically require preauthorization for procedures performed in an emergency room, observation unit, urgent care center, or during an inpatient stay.
Preauthorization requests should be submitted using the appropriate codes. Click here for a list of the CPT and HCPCS radiology codes requiring prior authorization in 2024 (Source: State of IOWA Department of Health and Human Services).
Challenges Involved
Radiology prior authorization requests are usually submitted and obtained by the referring physician, though some plans allow the radiology practice to do this. This also depends on state regulations.
While obtaining prior approval quickly is crucial to provide timely care, the process is complicated. In radiology, prior authorization processes that delay approval for imaging tests such as CT, ultrasound (US), MRI, PET, and single-photon emission computed tomography (SPECT) can significantly delay care for cancer patients.
Reports indicate that authorization-related issues are among the top reasons for claim denials. In a 2021 AMA prior authorization (PA) physician survey:
- 93% of respondents said that prior authorization can delay access to medically necessary care.
- 34% of respondents said prior authorization has led to a serious adverse event for a patient in their care.
Other challenges associated with radiology prior authorization are:
- Different health plans have different rules with regards to prior authorization, and understanding these requirements is crucial.
- Insurance companies often change their rules and procedures, so staying updated is crucial.
- If prior authorization is required for a procedure but not obtained, the claim can be rejected by the health plan even if the procedure is medically necessary and would otherwise have been covered. In this case, the patient may end up paying for it.
- Authorization denials increase A/R days, require time and work to appeal, correct or overturn, and lead to revenue loss.
As the radiology insurance verification and authorization process can be time-consuming and complex, requiring consistent follow-ups, many radiology offices opt to outsource the task. Insurance verification specialists can help you implement best practices to improve the pre-approval workflow.
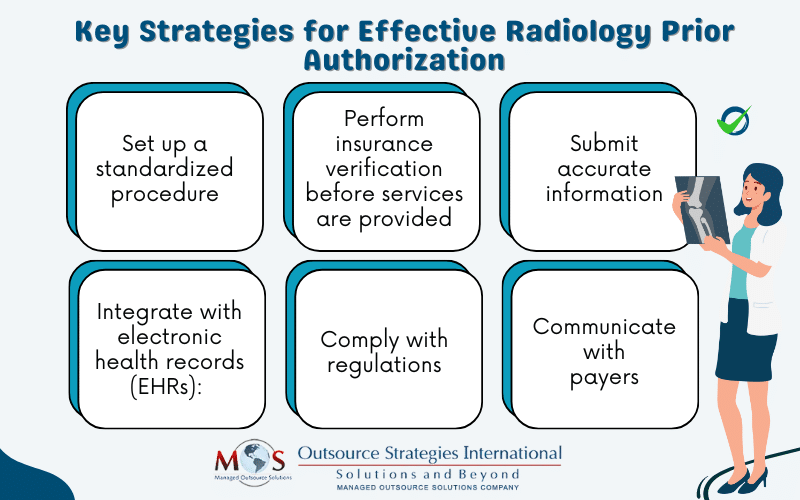
Best Practices for Radiology Prior Authorization
- Set up a standardized procedure: Set up a clear process for obtaining prior authorization, from verifying insurance coverage to submitting the prior auth request.
- Perform insurance verification before services are provided: Verify the patient’s coverage to determine benefits as well as prior authorization requirements. This will help you submit pre-approval requests in a timely manner.
- Submit accurate information: Ensure that the information you submit is accurate and thorough. This includes patient details and the appropriate CPT and ICD-10 codes. It is also necessary to submit documentation with the pertinent details supporting the medical necessity of the procedure. Mistakes in the request form or not submitting the request in a timely manner are common reasons for denials.
- Integrate with electronic health records (EHRs): Integrating the prior authorization process with EHRs can help streamline the process, ensuring that all necessary patient information is readily available.
- Comply with regulations: Ensure that your prior authorization process adheres to all relevant regulations, including HIPAA and state-specific guidelines.
- Communicate with payers: Collaborating payers can help streamline the authorization process for radiology services and get approvals on time.
Benefits of Working with an Insurance Authorization Expert
Partnering with a specialized radiology insurance authorization company is the best way to manage the time-consuming prior authorization procedure. Experts are well-versed in the applicable rules as well as matters like:
- Which procedures require authorization
- Which plans require prior authorization
- How to obtain the authorization
- Payer-specific rules: Medicare and Medicaid have specific requirements for prior authorization. Verification specialists are familiar with these rules and also up to date on payers’ changing rules and procedures related to prior auth.
Experts will directly communicate with insurance companies to verify and authorize procedures, reducing delays in patient care, boosting satisfaction among providers and patients, and improving reimbursement processes.