Pyogenic granuloma, also known as lobular capillary hemangioma or granuloma telangiectaticum, is listed by WHO under the range Diseases of the Skin and Sub-cutaneous Tissue. These are small, round, usually red-colored skin growths. They may bleed because they comprise a large number of blood vessels; otherwise they are benign lesions. They typically appear on the hands, arms, face, or mouth and are common in children and pregnant women.
Typically, pyogenic granuloma is diagnosed based on its appearance though a biopsy may be performed by the doctor for a more accurate diagnosis. This also helps rule out other cancerous conditions like squamous cell carcinoma, basal cell carcinoma, and melanoma. For doctors diagnosing and treating pyogenic granuloma, a physician billing service could provide significant support as regards medical coding and documentation.
ICD-10 Diagnosis Code for Pyogenic Granuloma
ICD-10 code L98.0 denotes Pyogenic granuloma. L98.0 is a billable/specific ICD-10-CM code that can be used on the medical claim to indicate a diagnosis for reimbursement purposes. Type2 excludes for this code include:
- pyogenic granuloma of gingiva (K06.8)
- pyogenic granuloma of maxillary alveolar ridge (K04.5)
- pyogenic granuloma of oral mucosa (K13.4).
Treatment Procedures for the Condition
Generally, physicians treat or remove factors that are expected to trigger the condition and thereby minimize the risk of its recurrence. Methods adopted include stopping any drugs that could activate the condition, advise proper oral hygiene, provide treatment for any oral trauma caused by the teeth and so on. Topical treatments provided may include cryotherapy, intralesional steroid injection and topical creams. Procedures include surgical excision, laser treatment, curettage and cautery. Excision treatment is credited with the lowest rate of recurrence (PubMed Central article). Health insurers may consider removal of benign lesions like Pyogenic granuloma medically necessary if any of the following criteria is met.
- Biopsy indicates pre-malignancy or malignancy
- The lesion’s anatomic location makes it vulnerable to repetitive irritation or trauma (for e.g. waist band, bar line, etc.)
- The lesion appears to be pre-malignant or malignant
- Lesions are causing symptoms such as bleeding, intense itching, burning, or irritation
- The lesion has evidence of inflammation such as erythema, edema, or purulence
- The lesion is infectious
- The lesion restricts vision or obstructs a body orifice
In the absence of the above indications, the removal of a benign skin lesion is considered cosmetic and non-reimbursable.
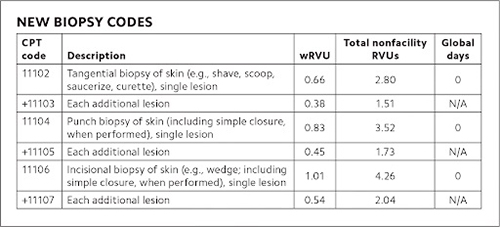
Procedure Codes Applicable to Removal of Pyogenic Granuloma
Pyogenic granuloma is a benign skin lesion that can be treated by excision. However, proper medical record documentation is necessary to establish why excisional removal other than for cosmetic purposes was the surgical procedure of choice. The code selection is determined by measuring the maximum clinical diameter of the apparent lesion plus that margin required for complete excision (the excised diameter is the lesion diameter plus the narrowest margins required). The margins indicate the narrowest margin required to properly excise the lesion based on the treating physician’s judgment. Each medical claim must be submitted with the appropriate ICD-10 code that shows the condition of the patient, and also indicate the reason for which the service was performed. Here are the CPT codes that can be used with a L98.0 diagnosis code for Pyogenic granuloma.
- 11300 ‐ 11313 Shaving of epidermal or dermal lesions
- 11400 ‐ 11446 Excision, benign lesions
- 17110 ‐ Destruction, (e.g. laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement) of benign lesions other than skin tags or cutaneous vascular proliferative lesions. This code is to be reported with one unit of service for removal of benign lesions other than skin tags or cutaneous vascular lesions, up to 14 lesions.
- 17111 – Destruction (e.g. laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement), of benign lesions other than skin tags or cutaneous vascular proliferative lesions. This code is to be reported with one unit of service representing 15 or more lesions.
The excision code typically includes anesthesia and simple closure. However, if the procedure involved extensive undermining, 2-layer closure and removal of excess skin, a separate code for moderately complex closure must be used.
Physicians Can Utilize Medical Billing Services
Medical coding and documentation for pyogenic granuloma is made challenging because of the many requirements the physician or medical coder must keep in mind when reporting a particular procedure code. For instance, excision codes include simple wound repair and so this shouldn’t be reported separately. When coding for wound closure or repair, the clinical documentation must support the complexity of the repair (simple, intermediate, or complex), the length in centimeters of the wound closed, and the anatomic location of the laceration/wound. These variables are specified in the repair CPT code descriptors.
For instance,
12013 Simple repair of superficial wounds of face, ears, eyelids, nose, lips and/or mucous membranes; 2.6 cm to 5.0 cm.
12035 Repair, intermediate, wounds of scalp, axillae, trunk and/or extremities (excluding hands and feet); 12.6 cm to 20.0 cm
The size and location of each lesion as well as the type of removal must be clearly documented. A biopsy code may also be used when samples of one or more of a group of lesions are taken for diagnosis, even if these samples are completely excised.
Image Source:
Medical billing outsourcing companies can provide the support physicians are looking for to ensure accurate medical coding and claim submission to payers. Besides, professional medical coders assign only the latest relevant codes because they stay updated with all the additions, deletions and modifications made to the medical codes from time to time. The correct codes on the medical claims are vital to get paid for your services. So, make sure that your medical coding and documentation is flawless, reliable, and supports medical necessity.