AI applications are transforming the medical billing process, making it faster, more accurate, and less prone to errors. By leveraging machine learning algorithms and automation, AI streamlines tasks, expediting the billing cycle while minimizing human errors. AI-driven systems also can analyze vast amounts of data quickly, identifying patterns and trends that aid in optimizing billing strategies and improving reimbursement rates.

Liked learning about AI and automation?
Explore further insights on role of technology in medical billing in our resource section.
AI applications in healthcare billing are transforming the process, making it faster, more accurate, and less prone to errors. Automation eliminates the necessity for extensive manual labor, thereby minimizing overhead costs linked to administrative tasks. By requiring fewer resources for billing and coding, your practice can allocate resources more efficiently, potentially resulting in significant cost savings.
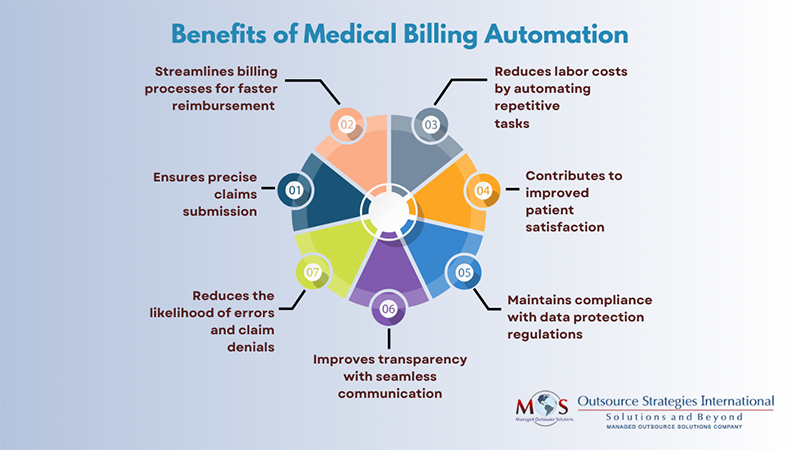
Benefits of Automation in Healthcare Billing
AI and automation in healthcare billing can revolutionize the traditionally time-consuming processes. The foremost advantage lies in heightened efficiency, as automated systems eliminate the need for extensive manual labor, reducing errors and expediting billing cycles. This can accelerate reimbursement and help achieve substantial cost savings by optimizing resource allocation. Enhanced accuracy and compliance are intrinsic to automated systems, ensuring precise coding and adherence to ever-evolving healthcare regulations. Predictive analytics offered by automation enable healthcare providers to proactively manage revenue cycles, identify trends, and address anomalies.
How Does Artificial Intelligence (AI) Transform Healthcare Billing in a Practice?
AI plays a pivotal role in streamlining and automating various facets of medical billing services, ranging from coding to seamless claim submission. Automation reduces the need for manual intervention, minimizing errors, and expediting the entire billing cycle.
Let us check out how artificial intelligence can improve the medical billing process.
- Automated coding: AI algorithms are adept at analyzing vast amounts of medical data, quickly and accurately assigning appropriate codes to diagnoses, procedures, and treatments. AI-powered software can analyze medical records and automatically assign appropriate codes, reducing errors and increasing efficiency. This can save time for professionals and reduce the risk of denied claims. The predictive capabilities of AI enable healthcare organizations to anticipate coding trends, identify potential issues, and proactively address them. The integration of AI in medical coding can enhance the precision of code assignment, accelerate the coding process, and contribute to the overall efficiency of healthcare RCM and reimbursement systems.
- Efficient patient appointment scheduling: Experienced medical coding and billing service providers already use advanced technology to help medical practitioners manage patient appointment scheduling and claims processing. Automating scheduling and sending appointment reminders to patients reduces the chances of missed appointments, driving efficiency and improving revenue cycle management. AI-enabled automated systems can help organizations track and improve performance on key healthcare metrics.
- Improve claims processing: AI aids in claims processing by automating the extraction of relevant information from medical records, ensuring accurate coding and reducing the likelihood of errors. The system can also predict potential issues that may lead to claim denials, allowing for proactive resolution. By automating these critical aspects of healthcare administration, AI not only increases operational efficiency but also contributes to a smoother and more patient-centric healthcare experience.
- Real-time patient eligibility verification: By using advanced algorithms and data processing capabilities, AI can automate the verification of patient eligibility and insurance coverage in a practice, reducing the likelihood of claim denials due to eligibility issues. AI systems can seamlessly integrate with electronic health records (EHR) and insurance databases, allowing for quick and accurate verification of patient eligibility for medical services. Through automated analysis, AI can instantly cross-reference patient details with insurance information, ensuring accuracy and completeness.
- Identifies billing trends and anomalies: AI algorithms can help practices uncover potential issues or areas for improvement. Through predictive analytics, AI can forecast potential RCM trends and identify anomalies that may indicate errors, fraud, or areas for improvement. This proactive approach allows for quick adjustments to billing strategies and better financial management. AI can also facilitate real-time claim adjudication by instantly reviewing claims for errors or missing information. This accelerates the reimbursement process and minimizes delays in revenue collection.
- Integration with Electronic Health Records (EHR): AI can seamlessly integrate with EHR systems, creating a unified platform for healthcare data. This integration streamlines the billing process, allowing for better coordination between clinical and billing information. Real-time updates between EHR and billing systems, facilitated by AI, guarantee that the billing information reflects the latest patient encounters, expediting claim submission and reimbursement. The adaptability of AI to changes in regulations ensures ongoing compliance and evolution with industry standards.
By incorporating these best practices, healthcare providers can optimize their AI-assisted medical billing processes, leading to improved financial outcomes, reduced administrative burden, and enhanced patient satisfaction.
AI transforms healthcare documentation and RCM in practices by introducing efficiency, accuracy, and proactive strategies, ultimately contributing to improved financial management and better patient care.


Learn about medical billing services and discover the impact of AI on billing efficiency.
Got questions? Call (800) 670-2809!