In healthcare, precise documentation is crucial, particularly for accurate medical billing. The careful recording and upkeep of detailed documentation is the foundation for maintaining financial integrity and efficiency in any healthcare system.
Accurate documentation by medical professionals, including patient data, diagnoses, treatments, and procedures, reduces the chances of claim denials and delays. Precise records ensure insurance companies have all the necessary details to process claims promptly, leading to faster compensation for healthcare professionals. The collaboration between accurate documentation and professional medical billing services creates a smooth financial ecosystem within the healthcare industry, benefiting both providers and patients alike.
Let us discuss the importance of documentation in billing, in detail.


Optimize your revenue today!
Explore our medical billing services for seamless financial health.
5 Reasons Why Accurate Documentation Is Crucial in Medical Billing
Clear and concise documentation is essential for ensuring accurate and timely payments for healthcare services.
- Clarity in patient care
Effective documentation is key to clear communication among healthcare providers. By capturing detailed and accurate patient information, medical practitioners ensure that the services rendered are clearly communicated, leaving no room for ambiguity or misinterpretation. This clarity extends beyond the clinical realm, directly impacting the accuracy of billing processes. Accurate claims and comprehensive documentation also help to establish trust with patients. Patients appreciate knowing that their healthcare details are documented with precision and in a secure manner. Trust in the healthcare facility leads to improved patient relationships and increased patient loyalty.
- Medical coding accuracy
The accurate translation of medical diagnosis, procedures and services into billing codes is a delicate process, heavily reliant on detailed documentation. Proper coding not only ensures that healthcare providers are reimbursed fairly for their services but also guards against potential audits or disputes. Documentation acts as the bridge, providing the necessary information for correct code assignment. Precisely matching diagnostic codes (ICD-10) and procedure codes (CPT) is crucial to align invoiced services accurately with the patient’s condition and medical procedures. This ensures accurate compensation and aids in maintaining accurate medical documentation. Accurate records provide essential data for precise programming, reducing the risk of coding errors.
- Reduces claim rejections and delays
When healthcare providers meticulously record patient information, treatment details, and the procedures performed, it ensures alignment with billing codes and correctly reflects the services rendered. This minimizes claim denials, and significantly enhances the chances of claims being approved upon submission to insurance entities. Partial or insufficient documentation may result in claims being rejected or processing delays. It is critical to make sure that all the essential data is made completely available. Omitted specifics or inadequate documentation may prompt inquiries from insurers. These might cause them to ask for more details or refuse the claim entirely. Accurate records reduce such concerns and ensure a streamlined workflow.
- Revenue cycle optimization
Documentation plays a pivotal role in optimizing the entire revenue cycle. From capturing patient demographics to detailing the services rendered and capturing diagnostic information, a well-documented process ensures a seamless flow of information. This, in turn, expedites the billing cycle, minimizing delays and facilitating prompt reimbursement. Accurate and complete documentation is essential for billing and revenue cycle management in healthcare organizations. Proper coding and billing rely on accurate descriptions of services provided, which are typically documented in the medical records. Accurate documentation acts as a guard against revenue leakage, which occurs when the services provided are not adequately captured or billed. Through comprehensive documentation, healthcare providers can identify and rectify potential gaps in the revenue cycle, ensuring that all services are accounted for and appropriately billed.
- Enhances auditing efficiencies
When medical professionals maintain precise records of patient encounters, diagnoses, treatments, and procedures, it creates a solid foundation for thorough audits. Clear and comprehensive documentation enables auditors to easily trace and verify the services provided, ensuring alignment with coding and billing standards. This approach also minimizes the likelihood of errors, discrepancies, or fraudulent activities. Thorough records allow for swift and efficient responses to audit inquiries, reducing the likelihood of penalties or fines and reinforcing the financial stability of healthcare institutions.

Check out an Overview of OSI’s Medical Billing Process!
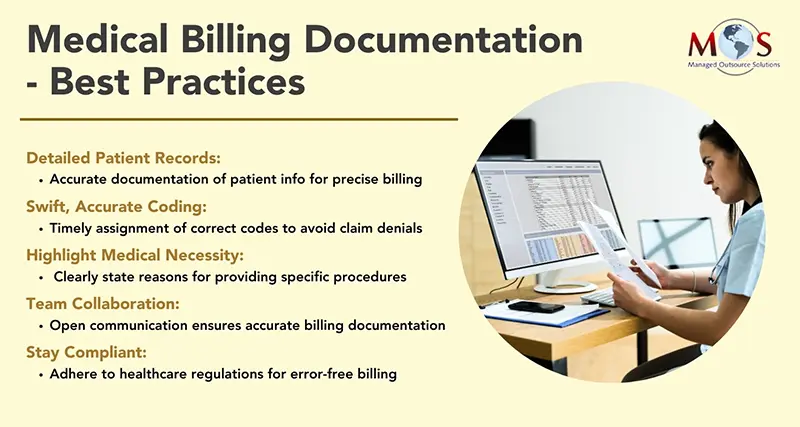
Optimizing Medical Billing with Documentation Best Practices
Adherence to best practices for medical billing documentation is paramount for ensuring accuracy, efficiency, and compliance. Comprehensive recording of patient information, including demographics and medical history, lays the groundwork for precise billing processes. Timely and accurate coding, regularly updated to meet industry standards, is essential in reducing the risk of claim denials and facilitating proper reimbursement.
Thorough documentation not only supports the legitimacy of the billed services but also facilitates clear communication with insurance providers, reducing the likelihood of disputes. Ensuring accurate records serve as a proactive measure, fortifying the entire claims submission process and ultimately contributing to a reduction in claim denials, thereby streamlining the financial operations of healthcare institutions.


Maximize your revenue potential!
Experience the ease and efficiency of our billing services!
Call (800) 670-2809