The current landscape of the healthcare industry is jam-packed with a plethora of challenges that necessitate practical and timely responses to provide quality care and secure fiscal stability. These include evolving billing standards, increasing patient expectations, and financial hardships encountered by medical practices. All these challenges can be addressed with a single solution: an efficient revenue cycle management (RCM) process.
According to Becker’s Payer issue, hospitals in the U.S. are estimated to lose up to $262 billion annually due to inefficient RCM systems. The intricate nature of revenue cycle processes requires optimization to ensure smooth operations and minimize revenue leakage. This is where RCM analytics plays an important role to streamline the entire process, from patient registration to final payment. With the help of medical revenue cycle management services, healthcare entities can identify billing errors, enhance collection efforts, and boost overall profits.
What Is Revenue Cycle Analytics?
Revenue cycle analytics refers to the data-driven insights prepared by healthcare organizations to gain valuable insights and uncover inefficiencies of the revenue generation system. It encompasses the gathering, analyzing, and reporting of a vast financial and operational dataset involved in the RCM processes to produce analytics reports.
Revenue cycle analytics primarily include the following types:
- Descriptive analytics
- Diagnostic analytics
- Predictive analytics
- Prescriptive analytics
- Denial management analytics
Healthcare providers use this RCM report to identify workflow bottlenecks, forecast revenue trends, and reduce billing errors. It allows practices to monitor their financial performance and enforce data-driven decision making to optimize their RCM system for better financial outcomes.
Types of Data Analyzed in RCM
Healthcare organizations utilize the following types of data in the analysis process, such as:
- Patient data: Comprehensive patient information such as demographic, insurance, and payment behavior details.
- Claims data: Detailed breakdown of claims data including denial rates, submitted claims, and reimbursement rates.
- Financial data: Profitability analysis of total collection rates, overhead expenses, and profit margin.
- Operational data: Information on the practice efficiency by analyzing coding accuracy, staff productivity, and patient satisfaction survey.
Key Steps of Data Analytics in RCM
Healthcare facilities can utliize data analytics for their revenue cycle process by implementing the steps given below:
- Collection: The foundational step that involves systematically collecting comprehensive data and identifying their relevant sources, such as EHRs, claims reports, and patient billing systems to ensure consistency and accuracy.
- Integration: Consolidating unstructured information from various sources into a single, unified dataset to be stored in a centralized repository for analysis.
- Quality assurance and analysis: Ensure data quality and accessibility by cleaning, processing, validating, and transforming datasets into standardized formats to eliminate errors and discrepancies. Perform the analytics process after verifying compatibility with the analytics tools to identify patterns, trends, and anomalies to drive evidence-based decision making.
- Actionable insights: Leverage valuable insights produced from the analysis by undertaking actionable strategies and initiatives to streamline billing processes, reduce denials, and enhance the overall cash flow of the practice.
- Continuous improvement: Establish a culture of continuous improvement by conducting regular audits, conveying the implications of analytics reports to stakeholders, and investing in staff training and education to foster transparency in communication.
Common Revenue Cycle Metrics Used in Data Analytics
The healthcare revenue cycle metrics provide valuable insights into financial performance, operational efficiency, and identifying practice inefficiencies. Given below are some of the most common healthcare revenue cycle metrics used in data analysis:
- Denial rate: The percentage of claims that are denied by payers compared to the total number of claims submitted.
- Charge capture rate: The percentage of charges for services rendered that are correctly captured and billed.
- Patient collection rate: The percentage of patient balances collected out of the total amount due from patients.
- First pass resolution rate: The percentage of claims that are paid on the first submission without needing rework or follow-up.
- Net collection rate: The percentage of the total amount billed that is actually collected, adjusted for contractual allowances and bad debt.
- Days in accounts receivable (AR): The average number of days it takes for a healthcare organization to collect payment after providing services.
Unlock the full potential of your practice by harnessing data-driven insights for your RCM process!
The Impact of Data Analytics on Revenue Cycle Management
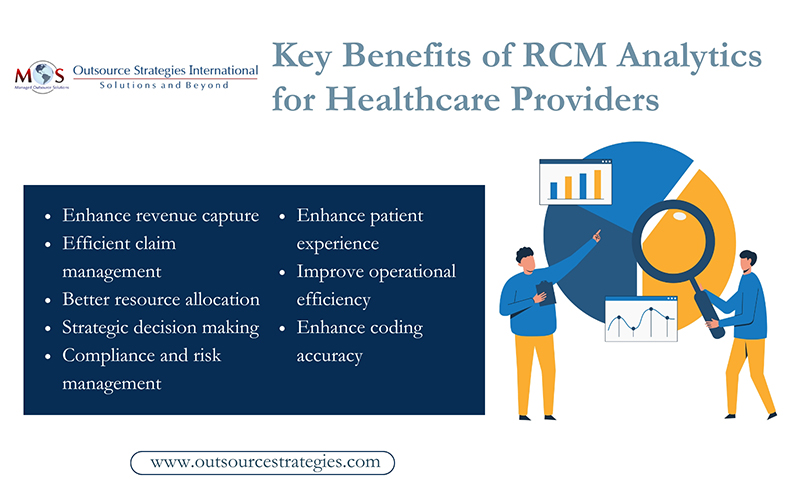
Healthcare providers can reap a number of benefits by leveraging the valuable insights generated by the RCM analytics process to optimize their billing system.
- Enhance revenue capture: Practices can significantly enhance their revenue capture by rectifying revenue leakage, identifying pitfalls in the billing process, and minimizing claim denials.
- Efficient claim management: Using analyzed data in healthcare organizations facilitates efficient claims management by reducing denial rates, uncovering root causes of denials, and identifying errors in claims. It can also predict the likelihood of denials based on past behavior. This results in first-pass adjudication rates and an overall improved success rate of submitted claims.
- Better resource allocation: By identifying obstacles, measuring workload, and monitoring productivity with RCA, practices can refocus their efforts towards areas with the greatest financial impact. This leads to better resource allocation within practices, fostering collaboration and productivity while minimizing waste, costs, and risks.
- Strategic decision-making: Data analytics allows healthcare leaders to make informed decisions based on real-time and predictive models for operational decisions impacting RCM, such as investment priorities, staffing levels, and cyber security measures.
- Compliance and risk management: Healthcare organizations face numerous regulatory requirements. Advanced revenue cycle analytics can help ensure billing and coding compliance, detect fraudulent activities, and identify unusual patterns in claims to protect the practice from malpractice and financial losses.
- Enhance patient experience: Healthcare providers use RCA to enhance patient experience through timely billing and transparent patient communication. This ensures higher patient satisfaction and retention rates. Practices can analyze patient behavior to predict payment patterns and offer patient-friendly options such as payment plans and automated payments to improve collections and reduce bad debt.
- Improve operational efficiency: RCA can contribute to operational efficiency by analyzing workflows, finding bottlenecks, and streamlining billing processes. It can pinpoint areas where automation could be applied, thus reducing manual errors, and freeing up resources for more complex tasks.
- Enhanced coding accuracy: RCA helps organizations monitor coding practices, flag coding errors in real time, and ensure that they are compliant with current regulations. By identifying coding errors early, practices can reduce the risk of costly audits and penalties.
Why Outsource Revenue Cycle Analytics to RCM Service Providers?
RCA has a transformative impact on healthcare RCM systems by furnishing practices with valuable insights and sophisticated tools to harness the power of data. By outsourcing the RCA process to medical RCM services, healthcare providers can leverage evidence-based knowledge to derive practical solutions. Healthcare organizations that integrate RCM data analytics can unlock substantial benefits such as streamlined operations, enhanced compliance, and accelerated payments. An efficient RCM system with data-driven strategies enables healthcare providers to render quality care, gain a competitive market edge, and strengthen financial stability.




