Healthcare receivables or accounts receivable (AR) in medical billing is the total amount of money owed to a healthcare provider by patients, insurance companies, or other payers for services rendered. In a complex environment with ever-increasing federal regulations, efficient AR management is challenging but critical to stay competitive. In fact, delayed, underpaid and denied claims are common issues that impact financial stability. The good news is that AR management is an important component of the services provided by a medical revenue cycle management company. Experts can help you implement actionable steps to collect balances and ensure that your AR stays healthy.
Optimize your medical billing process and maximize reimbursements with our professional AR management services.
The Growing Challenge of Claim Denials and Delayed Reimbursement on Healthcare Providers
Claim denials and reimbursement delays are a common problem. One survey found that more than 37% of healthcare providers are waiting for amounts ranging from $25,000 to $100,000, while another 32% are waiting to collect debts that exceed $100,000, according to a PYMNTS Intelligence report. The report further noted that The Working Capital Tracker® stated that 30% of healthcare providers say they have seen an increase in denial rates since the end of the pandemic.
According to data from over 1,800 hospitals and 200,000 physicians analyzed by Crowe Revenue Cycle Analytics, one in three inpatient claims submitted by providers to commercial insurers in the first quarter of 2023 went unpaid for more than three months. Additionally, 15% of both inpatient and outpatient claims were initially denied.
This post discusses the concept of AR, how reducing days in AR enhances financial performance, and strategies to improve healthcare receivables management.
Understanding AR Management in Medical Billing
The AR process begins when a healthcare provider either bills a patient or submits a claim to an insurance company. Once the patient pays the bill or the insurance company processes the reimbursement, the account is cleared from AR.
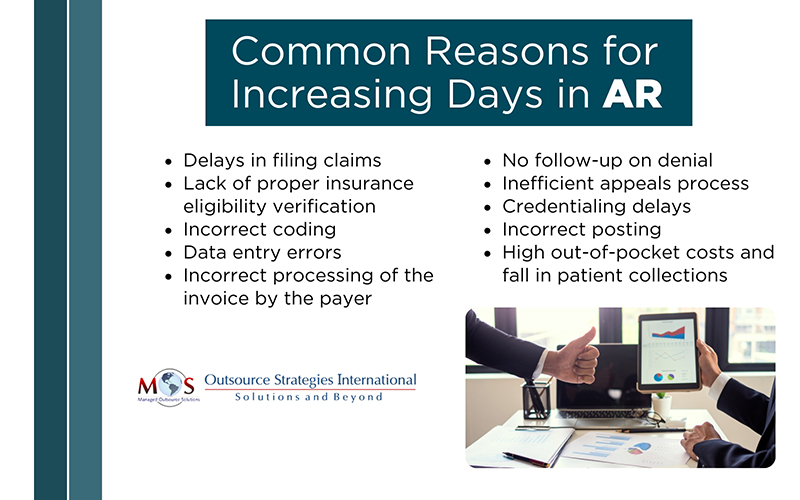
Ideally, a medical claim should be submitted within 72 hours after the service has been provided. Clean claims submitted electronically could be paid within two weeks. If your collections are getting delayed and overdue payments are piling up, it increases days in AR – the average time taken for a claim to be paid based on average daily charge volume. To assess your practice’s overall financial health and identify areas for improvement, you need to measure days in AR.
Days in AR is calculated by dividing the total accounts receivable by the average daily charges for your practice. The American Academy of Family Physicians (AAFP) recommends that Days in AR should stay below 50 days at minimum, though 30 to 40 days is preferable. Tracking Days in AR helps you understand how long it takes, on average, to collect payments so that you can take steps to improve collections and your revenue cycle.
Efficient healthcare receivables management ensures that you get paid in a timely manner.
Managing AR efficiently is an important element of billing success. AR management involves reducing days in AR by tracking unpaid accounts and taking steps to secure payments.
How Efficient Healthcare Receivables Management Works
Effective AR management in healthcare involves several key steps to ensure timely collection of payments and reduce denial rates.
- Proper Insurance Eligibility Verification
Accurate insurance information helps determine a patient’s coverage and financial responsibility. Insurance verification specialists verify details like insurance, demographics, and contact information before services are provided. This process confirms coverage, clarifies costs covered by insurance, and identifies patient payment obligations. Updating records before appointments ensures coverage confirmation and highlights any outstanding balances.
- Accurate Charge Capture
Accurately capturing all services and procedures performed is a crucial initial step in healthcare AR management within healthcare, where all services provided to a patient are accurately recorded and translated into billable charges. Clinicians and other healthcare professionals should accurately document the services delivered during a patient encounter in the electronic health record (EHR), which is then used for charge capture. By capturing all relevant details like procedures, medications, supplies, and diagnoses, charge capture directly impacts the accuracy of the patient’s bill, leading to timely and appropriate reimbursement.
- Clean Claim Submission
Timely and accurate claims submission to insurance companies is essential. Proper coding and complete documentation help avoid claims being rejected. Skilled medical coders will ensure that claims are submitted with the correct diagnosis and treatment codes and modifiers. Claims scrubbing is an important step in this context that helps ensure the claim contains all relevant details, and that there are no typographical errors, illegible content, or duplicate charges. Scrubbing helps to identify and correct errors, such as incorrect coding, missing patient information, or incomplete documentation. This reduces the risk of claim denials and delays. Claims scrubbing can also help to ensure compliance with regulatory requirements, such as HIPAA. Claims scrubbing technology is often used to help review claims for accuracy before they are submitted to insurance.
- Patient Financial Education and Follow-Up
After insurance payments are received, the remaining balances are billed to patients. Effective communication is vital for managing overdue accounts. Educate patients about their insurance benefits and out-of-pocket costs through a clear payment policy. Key policy elements should include payment due dates, responsible parties, handling of co-pays and deductibles, accepted payment methods, and details about fees, refunds, and collections. To reduce AR days, collect payments at service time, send timely payment statements, and provide multiple payment options. Regularly review patient aging reports, follow up on outstanding balances, and develop strategies for timely payers and those with larger dues.
- Payment Posting
Once payments are received from insurance companies and patients, they are accurately recorded in the patient’s account, ensuring reconciliation with outstanding invoices. This process ensures that patient accounts are updated in real-time, reflecting payments, denials, and any adjustments. Effective payment posting helps identify discrepancies such as underpayments, denials, or missing payments, enabling timely follow-up and corrective actions. Maintaining clear and organized payment records allows you to streamline their AR management, reduce outstanding balances, and enhance revenue cycle efficiency.
- Follow-Up on Denied Claims
AR specialists identify and correct reasons for denied claims, resubmitting them to secure payment for services provided. To ensure timely payments, identify and address issues delaying reimbursements. MGMA suggests analyzing collections by payer to spot slow-paying insurers and those with frequent denials. A medical revenue cycle management company can help you track payer reimbursements with monthly AR reports, showing amounts owed and uncollected. They also monitor claims to correct and resubmit denials or rejections.
- Reporting and Analysis
Regular analysis of AR data helps identify trends and issues, with metrics like aging reports essential for assessing billing efficiency. MGMA recommends that practices take note of repeated errors in gathering patient data, coding, billing, or other processes. These indicate the areas where changes need to be made.
Expertise Counts
Outsourcing AR management to specialized firms to reduce operational burdens. Efficient healthcare revenue cycle management services improve cash flow by helping providers collect payments faster. Experts often work with advanced software to automate tasks, reduce manual interventions for faster claim resolution, save time, and standardize processes to minimize errors. Proactive AR management identifies reasons for claim denials and corrects issues before submission, increasing the first-pass claim acceptance rate and reducing rework costs. By ensuring timely payments and reducing the risk of bad debt, AR specialists can improve healthcare revenue cycle efficiency, leading to increased returns on investment.
Partner with experts in medical revenue cycle management to boost cash flow and reduce payment delays.




