In any medical practice, timely reimbursement, financial stability, and the delivery of high-quality patient care depend on efficient medical claims submission and processing. Healthcare providers can enhance financial outcomes by deploying optimal strategies and using technology for an exceptional patient experience. Efficient claims processing in healthcare has long been associated with challenges such as prolonged reimbursement cycles, errors in coding, and complex regulatory compliance. These challenges affect the financial well-being of healthcare practices and impacts the overall patient experience. A reliable medical billing company can streamline the claims process, allowing healthcare practices to focus on patient care while optimizing their financial outcomes.
Some of the major challenges associated with medical claims submission and processing include:
- Coding errors: Even minor mistakes can lead to claim rejections and delayed reimbursements.
- Regulatory compliance burden: Failure to adhere to these regulations can result in penalties.
- Prolonged reimbursement cycles: Lengthy reimbursement cycles strain the financial resources.
- Inefficient workflow: Lack of efficiency in billing leads to delays in claim submissions.
- Limited technology integration: Lack of interoperability between systems hinders the seamless flow of information.
- Staff training and turnover: Ongoing staff training is crucial to stay abreast of coding updates.
- Insurance verification delays: Delays in insurance verification can hinder timely reimbursement.
Understanding and addressing these challenges head-on is crucial for healthcare practices aiming to streamline their medical claims submission and processing. Through a combination of advanced technology adoption, continuous staff training, and strategic partnerships with experienced medical billing companies, practices can navigate the complexities and achieve a more efficient and financially robust healthcare ecosystem.


Experience effortless claims processing!
Grow your practice with our cutting-edge medical billing services.
Call (800) 670-2809
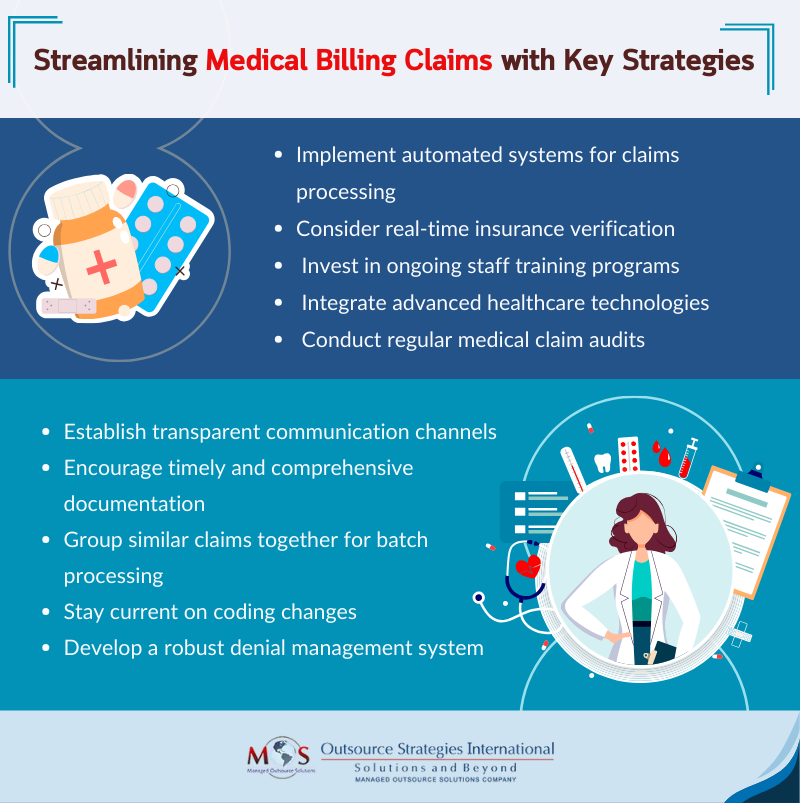
10 Best Practices for Healthcare Claims Submissions
Check out some of the best practices that healthcare practices can adopt to streamline their claims submission process, ensuring timely reimbursements and a smoother revenue cycle.
- Accurate patient information collection
Ensure thorough and accurate collection of patient information at the point of service. Precise details regarding demographics, insurance information, and contact details are crucial for preventing claim errors and rejections.
- Real-time insurance verification
Implement systems for real-time insurance verification to confirm coverage details before claim submission. This proactive approach reduces the likelihood of denials and accelerates the reimbursement process.
- Comprehensive staff training
Invest in ongoing staff training programs to keep your team updated on coding changes, regulatory updates, and the latest technologies. Well-informed staff members contribute to accurate claims processing.
- Utilization of technology
Use advanced healthcare technologies, including electronic health record (EHR) systems and claims management software. Automation can significantly reduce errors, improve efficiency, and enhance overall claims processing.
- Regular claims audits
Conduct regular audits of submitted claims to identify patterns of errors or issues. This proactive measure allows for the correction of systematic problems, reducing claim rejections and denials.
- Clear and transparent communication
Establish clear lines of communication between front-office staff, billing teams, and providers. Transparent communication ensures that everyone is on the same page, reducing misunderstandings and errors in claims processing.
- Timely documentation
Encourage healthcare providers to maintain thorough and timely documentation of patient encounters. Clear and comprehensive documentation is essential for accurate coding and supports the claims submission process.
- Claims batch processing
Implement batch processing for claims submission. Grouping similar claims together can streamline the submission process and optimize the use of resources, reducing manual workload.
- Stay updated on coding changes
Regularly update coding practices to comply with the latest industry standards and regulatory requirements. Staying current with coding changes helps prevent claim denials due to outdated codes.
- Efficient denial management
Establish a robust denial management system to quickly identify and address denied claims. Analyze denial trends to implement preventive measures and minimize future rejections.
Streamlining medical billing claims is paramount for the financial health and operational efficiency of healthcare practices. By adopting these best practices, healthcare practices can navigate the complexities of claims processing, reduce errors, and ensure a more streamlined revenue cycle. Practices are employing a combination of coding and revenue cycle management (RCM) services to ensure the initial accuracy of claim codes. This approach enables the submission of clean claims with correct codes and modifiers, enhancing the overall claims process. Leveraging AR follow-up services aids in identifying recurring issues and patterns, such as sending claims to the incorrect payer address or omitting payer-specific requirements on claims. It also helps detect consistent denials and more.
Ultimately, these measures contribute to enhanced financial stability and the ability to provide exceptional patient care. Choosing an experienced medical billing company with a proven track record, advanced technology integration, and a commitment to accuracy in medical billing services is crucial for efficient claims processing, ensuring timely reimbursement and financial stability.


Optimize your revenue cycle!
Consider our expert medical billing services for precision, speed, and financial success.
Call (800) 670-2809