Efficient DME insurance verification and authorization is essential in healthcare settings, since these devices take care of myriad health issues or physical conditions faced by patients.
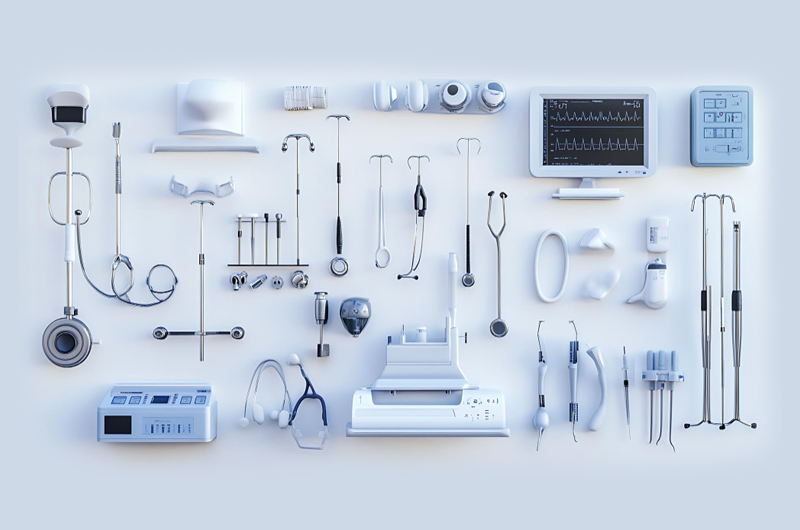
As you know, DMEs (Durable Medical Equipments) are medical devices that are needed to provide therapeutic benefits to the patient who is suffering from some illness or medical condition. Wheelchairs, prosthetics, orthotics, implantable devices, neurostimulators, oxygen and respiratory equipment, implantable devices, commode chairs, crutches, blood sugar monitors, etc are examples of DME.
DME is to be used at the residences of patients and can only be prescribed by a doctor. For securing reimbursement, the doctor must ensure that the patient is covered for the required equipment.
Insurance Verification
Verification is a very important process that precedes administering the DME. The process involves the following steps:
- Verifying in detail the medical coverage of the patient for ensuring coverage of the equipment and the related procedure
- Contacting the authorization department of the insurance companies
- Meeting the specific requirements of insurance companies to secure authorization of DME
- Getting the requirements submitted to the insurance company
- Following up every 24 hours with the insurance company till authorization number is received
- Recording the received authorization number in software for ensuring that the billed claim includes authorization number with everything properly reimbursed
Medicare Part B Covering DME
Medically required durable medical equipment that is prescribed to be used in the patient’s home is covered by Medicare Part B. This includes, though not limited to:
- Blood sugar monitors
- Blood sugar or glucose test strips
- Air-fluidized beds, other support surfaces
- Continuous passive motion (CPM) machine
- Canes excluding white canes for blind individuals
- Infusion pumps and supplies, when required for administering some drugs
- Manual wheelchairs and power mobility devices
- Crutches
- Hospital beds
- Commode chairs
Individuals with Part B Medicare are eligible for DME coverage. They need to pay 20% of the amount approved by Medicare. The Part B deductible is applied.
Reasons behind Inappropriate Payment
Some of the usual causes of inappropriate payment to providers can be attributed to unnecessary utilization of DMEs and insufficiency of supporting documentation. Some of the DME services could be non-covered or not allowed, which results in payment being withheld.
The complex nature of DME utilization makes it necessary to outsource DME insurance verification and authorization, to be on the safe side. Unpaid services could really hamper the bottom-line of physician practices, nursing homes and hospitals, so this is one aspect that must be handled professionally. The solution lies in either hiring experienced coders and setting up high tech verification systems, or outsourcing the process.