The challenges confronting the US healthcare system range from high costs to accessibility problems. The federal government introduced the value-based care strategy to improve the healthcare system in terms of outcomes, quality, equity and cost of care. Value based care links reimbursement for services provided to patients to the results delivered. It is a transformational shift from the fee-for-service paradigm, in which healthcare providers are paid for the amount or volume of services they provide – even if they don’t achieve the desired results.
As a highly experienced medical billing company, we stay updated on the emerging trends in medical billing. In this post, we explore the impact of value-based care on medical billing.

Medical Billing in the Value-based Care Scenario
Traditional fee-for-service models reward the quantity of services rendered, focusing on treating medical conditions as they occur. For instance, a patient’s annual check-up with a primary care physician involves various services like examinations, tests, and advice. After the visit, the provider bills the patient’s insurance or the patient directly for each service separately, like consultations, tests, procedures, and medications. Payments are made based on the services provided, following a set fee schedule, irrespective of how the patient’s health progresses.
In a value-based billing scenario, healthcare providers are compensated based on the quality and effectiveness of care delivered, rather than on a fee-for-service basis. Consider a value-based care arrangement between a healthcare provider and an insurance company for managing patients with diabetes. The physician creates a thorough care plan involving check-ups, screenings, lifestyle guidance, and specific health goals. Instead of billing for individual services, the provider gets paid based on how well they achieve outcomes like target blood sugar levels or reduced complications. The insurance company compensates the provider according to these outcomes, offering bonuses for success but potentially reducing reimbursements if benchmarks aren’t met. This system encourages ongoing patient monitoring and care coordination while incentivizing improved patient health results.
As physicians focus on mastering the value agenda, they need proper billing strategies for value-based care.
Assessing the Impact of Value-Based Care on Healthcare Billing
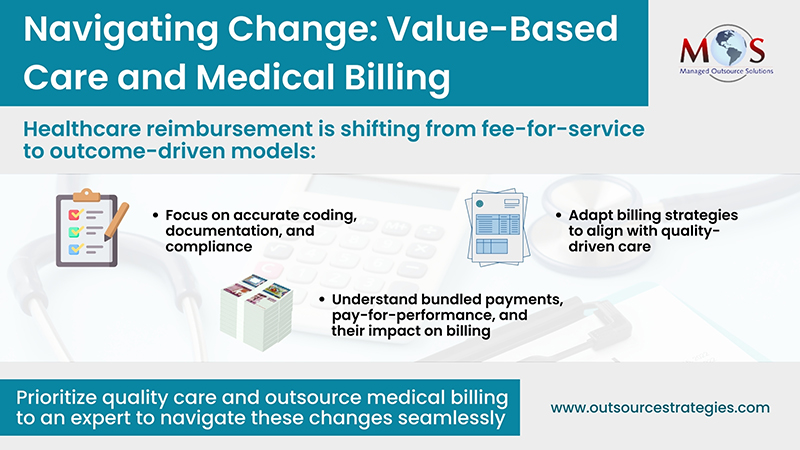
Implementing value-based care billing requires numerous changes in the conventional approach to revenue cycle management (RCM):
Precise CPT coding
The CPT code set plays a crucial role in advancing value-based care. Value-based payment models demand greater accountability. Ezequiel Silva III, MD, the past co-chair of the AMA Digital Medicine Payment Advisory Group, emphasizes the growing significance of the CPT code set for precisely detailing medical services provided in the value-based care scenario (ama-assn.org). To secure reimbursement, physicians need to report the correct CPT codes to describe the medical services and procedures delivered.
Outcome prioritization
Shifting from service quantity to outcome quality, clinicians must diligently track and report patient outcomes for accurate reimbursement.
Increased reporting requirements
Participation in value-based care necessitates specific quality measure reporting or engagement in alternative payment models, necessitating additional documentation for the billing process.
Enhanced care coordination
Value-based care streamlines communication and collaboration among clinicians, optimizing patient care and billing precision.
Billing for bundled services
A bundled payment is one form of value-based payment. It is a set price for a specific care period, often covering a procedure and all associated services for a medical condition. As the payment isn’t based on the quantity or variety of services provided, it encourages providers to coordinate care for better efficiency and quality across all included services. Bundling involves using a single CPT code to depict two distinct procedures carried out simultaneously. With both government and commercial health plans using bundled payments, knowing how to bill for bundled services is essential. Generally, bundling regulations dictate that if a minor procedure coincides with a more significant one, the code for the major procedure should be applied, for e.g., if needle insertion is part of a more complex medical procedure, only the CPT code for the this procedure should be applied.
Unbundling occurs when separate procedures that should be billed together under a single code are instead billed separately. This fraudulent practice inflates costs and can lead to overpayment by payers. Therefore, understanding bundling is crucial to avoid medical billing fraud.
Shared savings structures
In value-based care, some programs utilize shared savings models. These models involve a setup where healthcare providers, like hospitals or medical practices, share in the financial savings achieved through improved patient outcomes and cost-effective care delivery. Clinicians must understand these models and their impact on reimbursement.
How Medical Billing Services can Help
To sum up, value-based care will significantly impact medical billing by shifting the focus from volume-based reimbursement to outcomes-based payments. Billing will increasingly depend on the quality and effectiveness of care delivered rather than the quantity of services provided. This transition will involve new payment models, such as bundled payments or capitation, emphasizing accurate documentation of outcomes, incentivizing preventive care, and encouraging cost-effective, high-quality care delivery.
Outsourced medical billing services can play a crucial role in adapting to the changes brought by value-based care. Medical billing experts can implement proper billing strategies for value-based care, enabling healthcare providers to focus on delivering high-quality patient care while ensuring appropriate reimbursement for services rendered.
Experienced companies can help providers navigate the complexities of new payment structures, such as bundled payments or pay-for-performance models. For instance, while EMR/EHR systems automate claims, we meticulously review them prior to submission. The automation often overlooks vital details such as modifiers crucial for claim approval. Additionally, our clients entrust us with their verification process to inform patients of their full financial obligations before appointments.
Boost medical coding accuracy and efficiency!


Stay ahead of the curve and prioritize quality care while we handle your billing needs!
Call Now (800) 670-2809