Utilizing the right medical modifiers are a crucial part of the medical billing process. Knowing how to use CPT code modifiers correctly helps drive proper reimbursement. These two-character additions to CPT codes provide additional information about the performed procedure, such as changes in circumstances, the extent of the service, or special conditions that affect how the service is billed. Modifiers are appended to CPT codes to convey to the insurance company that the service was altered in some way from the stated CPT descriptor without changing the definition. Partnering with a professional medical coding company can ensure accurate modifier usage, reducing the risk of claim denials and optimizing revenue.
Simplify your billing process and boost reimbursements with our expert medical coding services.
Understanding and appropriately using CPT modifiers can make the difference between a clean claim and a denied or delayed payment. This blog explores what CPT code modifiers are, their purpose, and how they help bridge the communication gap between healthcare providers and payers. This guide aims to provide clarity on how these modifiers are used to enhance claim accuracy and compliance.
Types of CPT Modifiers
CPT codes are primarily used in office and outpatient settings to report medical procedures and services in claims submitted to insurance companies. These codes are assigned based on the physician’s documentation in the medical record. Modifiers provide a way to convey specific circumstances related to how a procedure or service was performed.
The two broad types of modifiers used in medical billing are:
- Level I Modifiers – Level I CPT modifiers consist of two digits and are maintained by the American Medical Association (AMA).
- Level II Modifiers – Level II modifiers or HCPCS modifiers are alphanumeric or have two letters and maintained by the Centre for Medicare & Medicaid Services (CMS).
Specifically, a modifier provides the mechanism to:
- Communicate additional information to payers, such as alterations, special circumstances, or exceptions in the delivery of care, without changing the core definition of the CPT or HCPCS code.
- Provide additional information about a service that has been performed more than once or services that have occurred unusually.
- Provide information not included in the code descriptor.
- Provide additional context or detail required by certain insurance companies or payer programs.
According to CPT, the situations when the use of a modifier may be appropriate are:
- The service or procedure has both professional and technical components
- More than one provider performed the service or procedure
- More than one location was involved
- A service or procedure was increased or reduced in comparison to what the code typically requires
- The procedure was bilateral
- The service or procedure was provided to the patient more than once
Commonly Used Medical Billing Modifiers
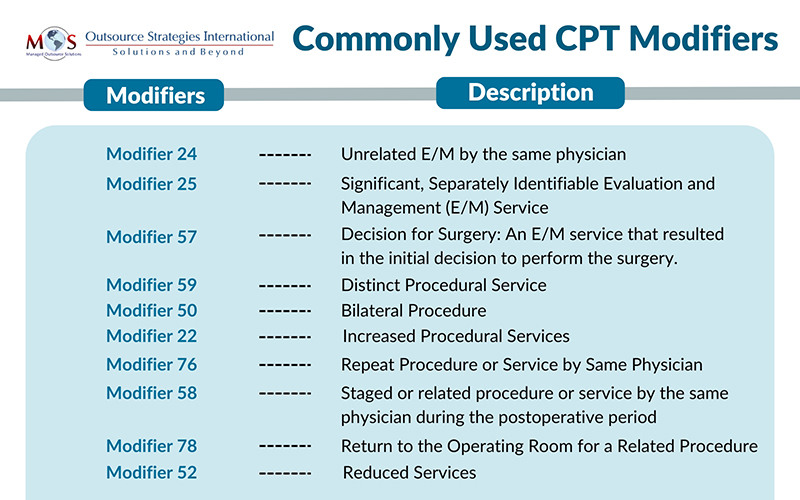
The following are some of the frequently used CPT modifiers:
Modifier 24 – Unrelated E/M by the same physician
An E/M service provided during the global period of a procedure is typically not separately reimbursed; instead, it’s bundled into the payment for the procedure. The exception to this rule is when the E/M service is unrelated to the procedure.
Modifier 24 Unrelated E/M by the same physician or other qualified health care professional during a postoperative period indicates that the E/M service being billed is not part of the global surgical package and, therefore, is separately reimbursable.
Example: A patient develops a skin infection after a rhinoplasty; the E/M service for treating the infection should be billed with Modifier 24.
Modifier 24 should be appended only to E/M codes.
Modifier 25 – Significant, Separately Identifiable Evaluation and Management (E/M) Service
This modifier is appended to office visits the same day as a minor surgery (0 or 10-day global period) when they meet the definition of significant, separately identifiable E/M service by the same physician on the same day of the procedure or other service.
Example: A patient comes in for a routine follow-up visit for their chronic condition (e.g., hypertension). During the visit, the physician also takes a detailed history and performs a thorough examination regarding a separate, unrelated chronic medical condition that the patient mentions. A minor surgery is also performed to remove an ingrown toenail. This additional E/M service could be considered “separately identifiable” and billed with a modifier 25.
Modifier 57: Decision for Surgery: An E/M service that resulted in the initial decision to perform the surgery.
Modifier 57 applies when the physician determines the need for any major procedure—whether surgical or non-surgical. CMS defines a major procedure as any procedure with a 90-day global period, as determined by the Medicare Physician Fee Relative Value File.
Appending modifier 57 to an E/M code alerts the payer that the E/M service—on either the day of, or the day before, a major surgical procedure—was the service at which the physician determined the surgery was appropriate and medically necessary, and is therefore not bundled to the surgery payment.
Example: A surgeon sees a patient and determines (and appropriately documents) that patient needs an emergency appendectomy. Because the E/M led to the decision for surgery, both the E/M (with modifier 57 appended) and the surgery may be reported, with separate payment for each.
Modifier 57 can be used on any E/M service—office visit, ED visit, initial hospital service, or critical care service.
Modifier 59 – Distinct Procedural Service – Indicates that a procedure or service was distinct or independent from other services provided on the same day.
This modifier is used to prevent bundling. When applied correctly, it enables the physician to report and receive payment for two or more procedures that would typically not be billed or reimbursed separately during the same provider/patient encounter. Modifier 59 is applied to indicate the following:
- Different encounter or session
- Different procedure or surgery
- Different site or organ system, or
- Separate incision, excision, injury, or lesion
Example: A patient who undergoes a colonoscopy (CPT code 45378) and also requires a biopsy (CPT code 45380) for a distinct lesion identified during the procedure. Modifier 59 is appended to the biopsy code to show that it is a distinct and separate procedure from the colonoscopy, and not part of the same bundled service.
According to the Office of Inspector General, Modifier 59 is frequently overused and misapplied. Before applying this modifier, coders must ensure that the documentation supports the separate status.
Modifier 50 – Bilateral Procedure – Used when a procedure is performed on both sides of the body during the same session.
Example: A patient requires a bilateral mastectomy. The physician performs the procedure on both breasts during the same surgical session. Adding Modifier 50 to the mastectomy CPT code indicates that it was a bilateral procedure.
Modifier 22 – Increased Procedural Services – Used when the complexity of a procedure is significantly greater than the usual level of service.
Example: A patient requires a complicated knee arthroscopy due to unexpected extensive damage to the joint. If the surgeon performs an extensive procedure that requires extra time and effort, Modifier 22 is used to indicate that the complexity of the procedure exceeded the usual level of service. The surgeon may request additional reimbursement for the increased work.
Modifier 76 – Repeat Procedure or Service by Same Physician
Indicates that a procedure or service was repeated by the same physician on the same day.
Example: A physician performs a wound debridement (CPT code 11042) on a patient. Later that same day, another round of wound debridement is performed due to further complications. Modifier 76 would be added to the second debridement code to indicate that it is a repeat of the initial procedure performed by the same physician on the same day.
Modifier 58 – Staged or related procedure or service by the same physician during the postoperative period
Append modifier 58 to the code for the subsequent procedure to indicate that it was performed during the postoperative period and was either: planned or anticipated (staged), more extensive than the original procedure, or necessary for therapy following a diagnostic surgical procedure.
Regardless of whether the procedure was planned or unplanned, it is always performed to address the original underlying condition, rather than as a result of the previous procedure. The key to using modifier 58 is that it typically applies to a procedure that the physician expected to perform before the completion of the initial surgery. A new global period begins with each subsequent procedure, and generally, there is no reduction in reimbursement.
Modifier 78 – Return to the Operating Room for a Related Procedure
Used when a patient requires an unplanned return to the operating room for a procedure related to the initial surgery. Here’s an example:
Example: A patient undergoes a laparoscopic gallbladder removal (cholecystectomy – CPT code 47562). During the recovery phase, the patient develops a bile leak, which is a complication resulting from the initial surgery. To correct this issue, the same surgeon returns the patient to the operating room within the global period of the original surgery to perform a drainage procedure to resolve the bile leak.
Unlike modifier 58, which indicates a subsequent procedure aimed at treating the same condition as the original surgery, modifier 78 is used for an unplanned related operation. This modifier applies when the same provider returns to the operating room (OR) during the global period of a previous procedure to address a problem or complication resulting from the initial surgery.
When modifier 78 is appended to a code, only partial reimbursement is typically provided, based on the insurer’s guidelines. This is because codes with modifier 78 usually receive payment for the intra-operative portion of the service only.
Modifier 52 – Reduced Services – Indicates that a service was partially reduced or eliminated at the physician’s discretion. It applies when the provider performs a service but does not complete it to the full extent described in the CPT code. This modifier helps ensure appropriate billing by notifying the payer of the reduced scope of the service.
Example: A patient undergoes a diagnostic colonoscopy (CPT code 45378) to examine the entire colon. However, due to poor bowel preparation, the physician could only advance the scope to the sigmoid colon and could not complete the full procedure.
Appending modifier 52 to CPT code 45378 indicates that the colonoscopy was not completed to the cecum but was partially performed.
Ensuring Correct Modifier Usage
As modifiers provide crucial information about a claim, they can significantly impact reimbursement. However, selecting the correct modifier can be challenging, particularly when multiple modifiers have similar descriptions. Moreover, modifiers are occasionally updated to reflect changes in medical practices, coding guidelines, and payer requirements. Partnering with professional medical billing and coding services is a practical way to ensure proper use of modifiers, stay updated with changes, avoid costly errors, and optimize reimbursement.
Partner with us for reliable medical coding solutions! Ensure your claims are compliant and error-free!




