The D2950 dental code is used to describe a “Core Buildup, Including Any Pins” in dental procedures.
D2950 – Core Buildup, Including Any Pins
A core buildup is necessary to provide a stable foundation for a dental crown or other restorative work. Billing code D2950 is often a challenge. Being an experienced Dental Insurance Coordinator, I have a strong feeling that most dental practices don’t even know when it is appropriate to bill or not for buildup. Dental practices also have to take effort to make their patients understand the limitations of their plan prior to treatment to avoid any further issues. So, here are some details on the topic which would be helpful to dentists as well as dental billing companies.
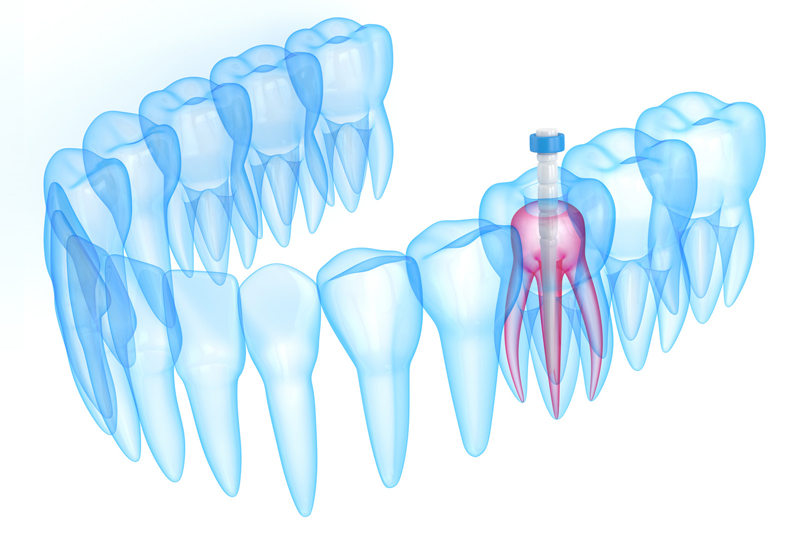
The D2950 code refers to the reconstruction or buildup of a tooth’s core structure, typically involving the placement of materials to support a dental restoration (such as a crown) when the existing tooth structure is compromised. It may include the placement of pins or posts to enhance stability. This code is used when a tooth has lost a significant portion of its structure due to decay, trauma, or other factors.
Dental insurance plans may cover a portion of the cost associated with D2950, depending on the patient’s policy and the necessity of the procedure. While certain carriers reimburse patients for buildups only in cases of previous endodontic treatment, some will provide a benefit if the remaining anatomical tooth structure can be described as less than 50 percent and inadequate to provide proper crown retention. It is crucial that the most accurate code is reported, whether the coverage exists or not.
Improve the accuracy of your dental core build-up coding with OSI’s dental coding services.
Call us at (800) 670-2809!
When Insurers Deny CDT Code D2950
Insurers will not reimburse for core buildup –
- if the procedure is billed on the same day as a root canal, as it will be considered inclusive of the root canal fee.
- if the procedure involves a clean or ideal crown prep. If a posterior tooth undergoes endotherapy, the restorative dentist would then perform a pre-fab post and core (D2954) or indirect post and core (D2952). The most common is the pre-fab post and core (D2954). Payers will usually reimburse for a D2954 even if you bill for an indirect post and core (D2952).
- if the claim lacks a benefit narrative from the dental office. Benefit narratives are concisely written dental-medical necessity statements to prove why the care was performed. An increasing number of dental carriers are recognizing the medical nature of certain dental procedures. All dental practices should document dental-medical necessity routinely to help optimize dental benefit coverage and cross-coding opportunities. According to Dentistry iQ, the narrative might read like, “Endodontically treated xx/xx/xx. 65% tooth structure missing. Needed for crown retention.”
- If the code is overutilized: Some dental insurance plans have limitations on the frequency or circumstances under which they will cover a core buildup. For example, they may only cover it if the tooth meets specific criteria, such as extensive damage or the need for a crown. Overutilization occurs when this specific code is billed more frequently than what is clinically necessary. When a code is used too much or overutilized, it is frequently dropped from insurance plans, leading to denials. Make sure not to use this code for fillers (see D2949) or bases (included in restorative procedure itself).
Other reasons why insurers may deny code D2950:
- Preauthorization requirements: Insurers often require preauthorization or prior approval for certain dental procedures, including core buildups. Failure to obtain preauthorization can result in a claim denial.
- Documentation errors: Inaccurate or incomplete documentation submitted with the claim can lead to denials. It’s essential for dental providers to ensure that all necessary supporting documentation, including X-rays and treatment notes, is included.
- Policy exclusions: Some dental insurance plans have exclusions for specific procedures or treatments, and core buildup may fall under such exclusions in certain cases.
- Benefit year limitations: Dental insurance plans typically have benefit year limitations, which means they may cover a core buildup once in a specific time frame (e.g., once every five years). If the patient has already had a core buildup within that period, the claim may be denied.
- Alternative treatment options: Insurers may deny a core buildup if they believe that a more conservative or cost-effective treatment option is available.
- Lack of medical necessity: Insurers may require that a core buildup is medically necessary, meaning that the tooth’s condition justifies the procedure. If they determine that it is not medically necessary, they may deny the claim.
It’s important to note that the specific use of dental codes like D2950 may vary depending on the patient’s individual dental condition and the treatment plan recommended by their dentist.
Other buildup codes – D2952 and D2954
D2952 is Cast Post and Core, in Addition to Crown. It differs from D2950, which refers to a laboratory cast post that is cemented into an endodontically treated tooth to build up the anatomical crown prior to a crown preparation. Core material also is used. However, most carriers will not pay for a D2952 and a D2950 on the same tooth.
D2954 is Prefabricated Post and Core, in Addition to Crown. This procedure includes the core material and the code describes a “store-bought” post that is typically used to build up an endodontically treated tooth. Claims using this code should include a narrative noting that the tooth has been endodontically treated and that less than 50 percent of the tooth structure is remaining.
D2950 vs. D2949
Based on CDT 2014 descriptor, D2950 “Refers to building up of coronal structure when there is insufficient retention for a separate extracoronal restorative procedure.” According to ADA, Core Buildup, Including Any Pins is referred to building up of the anatomical crown when a restorative crown will be placed, whether or not pins are used.
The core buildup (D2950) is commonly used incorrectly by many practices. The code (D2950) usually applies to teeth that do NOT have enough tooth structure to support a crown. Typically, 60% or more of the tooth is missing.
D2949 Restorative Foundation is a code in CDT 2014.
D2949 – Restorative Foundation
The CDT descriptor for D2949 is “Placement of restorative material to yield a more ideal form, including elimination of undercuts.” This code describes a procedure where restorative material is placed in the tooth for purposes other than helping the new crown stay on. This procedure is often incorrectly submitted as a D2950 buildup.
The procedure might include blocking out undercuts so impressions are easier to take, filling in voids in the prep, eliminating a box form, filling in a concavity or even making the shape of the prepped tooth more “ideal” in contour.
Tips to Minimize Claim Denials for Core Buildups
Here are some tips to minimize claim denials for core buildups:
- Provide clear documentation of the condition that resulted in the buildup in the initial claim submission. Make sure that the documentation indicates that the tooth was broken down to the extent that a buildup was necessary to perform the endodontic procedure.
- Provide supporting details along with the claim. Claim approvals from payers for core buildup require supporting X-rays. Attaching photos of the tooth being treated along with the claim also gives a better idea of how much decay existed, and it helps to speed up claim approvals.
- Submit an endo prognosis, a well-detailed narrative, and pre- and post-op radiographs to prove clinical necessity. Radiographs and intraoral photographs can be submitted as part of a narrative to the insurance carrier.
In cases of denial, the dental office must submit an appeal outlining the reasons for the procedure, leading to improved prognosis. Proper denial management is critical. A proper appeal involves sending the payer a written request to reconsider the claim. Additional documentation including radiographic evidence or a narrative description should be included to give the carrier a clearer picture of why the treatment was recommended.
Dental billing and coding comes with many challenges. A dental billing company can play a crucial role in ensuring that dental practices receive prompt and accurate reimbursement for their services while allowing dental professionals to focus on providing high-quality patient care
The D2950 dental code is used to describe a “Core Buildup, Including Any Pins” in dental procedures. Here’s some more information about this code:
D2950 – Core Buildup, Including Any Pins:
Definition: This code refers to the reconstruction or buildup of a tooth’s core structure, typically involving the placement of materials to support a dental restoration (such as a crown) when the existing tooth structure is compromised. It may include the placement of pins or posts to enhance stability.
Materials Used: Dental materials like amalgam, composite resin, or other restorative materials are used to rebuild the core of the tooth. Additionally, pins or posts made of materials like metal or fiber may be inserted into the tooth to provide additional support.
Associated Procedures: D2950 is often used in conjunction with other dental codes, such as those for crowns (D27XX) or posts and cores (D29XX), as part of a comprehensive restorative treatment plan.
Insurance Coverage: Dental insurance plans may cover a portion of the cost associated with D2950, depending on the patient’s policy and the necessity of the procedure.
Provider’s Recommendation: Dentists typically recommend a core buildup when they believe it is necessary to provide a stable foundation for a dental restoration. This procedure is essential for preserving the tooth’s structure and ensuring the long-term success of the restoration.
Patients should consult with their dentist and dental insurance provider for more information about the use of this code in their specific case.
Dental insurers may deny CDT code D2950, which represents a core buildup, for various reasons. It’s important to understand that insurance coverage policies can vary widely between different providers and plans. Here are some common reasons why insurers might deny this code:
Policy Specifics: The denial could also be due to specific policy details or interpretations made by the insurer. Each insurance plan can have unique terms, conditions, and definitions that affect coverage.
We code your dental procedures accurately, allowing you to focus on providing quality patient care.
Want more details regarding our services? Call (800) 670 2809!
Patients and dental providers can appeal claim denials if they believe the procedure is justified based on the patient’s dental health needs. This may involve providing additional documentation, explaining the medical necessity, or following the insurer’s appeals process.
It’s crucial for patients to review their dental insurance policy documents and discuss coverage and potential denials with their dental provider to better understand their benefits and options.