With the introduction of ICD-10 codes in 2015, physicians had to make major changes to documentation. What healthcare providers should keep in mind at all times is that it is documentation that gets coded. With good, comprehensive clinical notes, medical billing and coding service providers can ensure accurate ICD-10 coding which leads to appropriate and timely claims payments for hospitals and physicians.
Complete and Accurate Documentation for Correct ICD-10 Coding
ICD-10 coding set was developed to reflect the increase in complexity of medical documentation due to advanced procedures, new devices and other developments in medicine. The goals of through documentation are to:
- Ensure the details needed for patients to receive the best quality of care
- Provide the information needed to show that physicians and organizations provided quality care.
- Accurately reflect the severity of illness of the patient while utilizing terms recognized by the Centers for Medicare & Medicaid Services (CMS) that will ensure precise code assignment
- Provide more detailed information to other health care providers performing subsequent care or services on patients
As requirements for physician-specific data increase, clear documentation with correct ICD-10 coding could impact potential pay-for-performance programs. In the 2022 ICD-10 Guidelines, a new paragraph reproduces an excerpt from the introduction to the guidelines:
“As stated in the introductory section of these official coding guidelines, a joint effort between the healthcare provider and the coder is essential to achieve complete and accurate documentation, code assignment, and reporting of diagnoses and procedures. The importance of consistent, complete documentation in the medical record cannot be overemphasized. Without such documentation accurate coding cannot be achieved. The entire record should be reviewed to determine the specific reason for the encounter and the conditions treated”.
ICD-10 Concepts and Coding
Documentation should cover specificity, laterality, severity of disease, time of onset and so on. Let’s take a look at the concepts and coding guidelines in ICD-10 on these aspects:
Greater specificity: With ICD-10, there is need for more specificity within documentation in order to support the more detailed code set. Physicians should capture more specific information in the patient record so that coders can select the right ICD-10 code for a symptom, disease, or provided service. To take a basic example, ICD-10-CM codes are distinguished by severity:
- mild intermittent asthma (J45.20 – J45.22)
- mild persistent asthma (J45.30 – J45.32)
- moderate persistent asthma (J45.40 – J45.42)
- severe persistent asthma (J45.50 – J45.52)
This implies that instead of documenting “asthma,” the physician has to document the severity level of asthma.
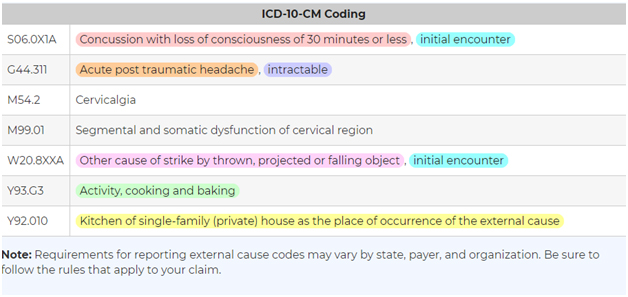
One often cited example is that provided by the AAPC, which describes the case of Mrs. Finley, who suffered a concussion when a cabinet fell on her head. She continued to suffer headaches (cephalgias). To document such a case, physicians will need to be specific. The documentation should include:
- the type of encounter
- applied specificity (whether the patient lost consciousness)
- acute or chronic condition
- relief or non-relief of symptoms
- the external cause of the accident
- the activity being performed
- the location where the accident took place
Taking these factors into account, AAPC provides the ICD-1o coding for this encounter
Unless the physician notes every single factor relating to the accident in the documentation, the coder cannot select the proper ICD-10 codes. With the greatest specificity in the documentation, the coder can identify the most accurate, applicable code, so that payer can provide accurate reimbursement for the consult.
Other Specified vs. Unspecified
An “other specified” or “other” code indicates that a specific code is not available for the condition documented in the medical record. If the documentation is not specific, coders may be inclined to assign an “unspecified” code. An “unspecified” code means that the condition is unknown at the time of coding. If more information is obtained about the patient’s condition, the unspecified diagnosis may be assigned a more specific code later.
Acute vs. Persistent vs. Recurrent vs. Chronic
Physicians should know how acute, persistent, recurrent, and chronic are defined for various diagnoses. ICD-10 guidelines define how many episodes within a period of time make up acute, persistent, recurrent, and chronic.
Laterality
Location matters. Clinicians and coders should indicate left, right or bilateral when appropriate. There are ICD-10 codes that indicate laterality, specifying whether the condition occurs on the left or right, or is bilateral. In ICD-10:
“1” represents the right side
“2” represents the left side
“3” means bilateral or both
For e.g., the ICD-10 codes for otitis media are:
H65.01 – Acute serous otitis media, right ear
H65.02 – Acute serous otitis media, left ear
H65.03 – Acute serous otitis media, bilateral
Payers may deny any codes that lack specificity when it comes to laterality. If laterality is not documented, reliable coders will query the clinician to get the missing information.
Tips for Writing Comprehensive Clinical Notes
AHIMA provides these simple guidelines to help clinicians ensure thorough and accurate documentation for correct ICD-10 coding:
- Know the basic principles underlying how codes are assigned based on documentation. Specify the patient’s condition correctly to ensure correct coding.
- Codes can be assigned for documentation by physicians, nurse practitioners and physicians’ assistants, but information in nurses’ notes cannot be coded.
- In outpatient coding, coders can code from the pathology and radiology reports without the attending/treating physician confirming the diagnosis. The pathologist and radiologist are physicians and if they have interpreted the tissue or test then it may be coded.
- The quality of clinical documentation and coding can be improved by delineation of cause-and-effect through the appropriate use of the phrases such as “due to” and “manifested by.”
- The “Principal Diagnosis” should be clearly stated. This is the condition established as being mainly responsible for the admission of the patient to the hospital. When the Principal Diagnosis is clear, the coder can identify it as the “First-Listed Diagnosis”.
- The physician should use terms such as “probable,” “suspected,” and “rule out” as appropriate when the diagnosis is inconclusive, though coding rules may differ between the inpatient and outpatient setting.
- Specificity is crucial when documenting radiologic and pathologic findings. Provide enough information so that the results can be properly and completely coded.
- Ensure details and specific information about procedures that are performed in any setting.
- For correct Hierarchical Condition Categories (HCC) coding, documentation must support the presence of the condition and indicate the provider’s assessment and/or plan for management of the condition. The diagnosis should have been Monitored, Evaluated, Assessed, or Treated (“M.E.A.T.”). This approach is valid and appropriate not only for reimbursements based on risk-adjustment but for all settings and payers.
Thorough documentation supported by appropriate coding of the patient’s problems will accurately reflect the overall condition of the patient. With the relevant components of documentation included in clinical notes, medical billing and coding outsourcing companies can help physicians ensure complete and accurate ICD-10 coding