In the realm of medical coding, anesthesia coding is a specialized branch that requires an understanding of the intricacies involved in anesthesia coding guidelines to provide an accurate charge capture. Unlike other services in which coding is based on the procedure performed, anesthesia differs as the coding is determined by various factors, such as:
- Medical Condition
- Type of Anesthesia
- Duration of Anesthesia
- Complexity of the Procedure
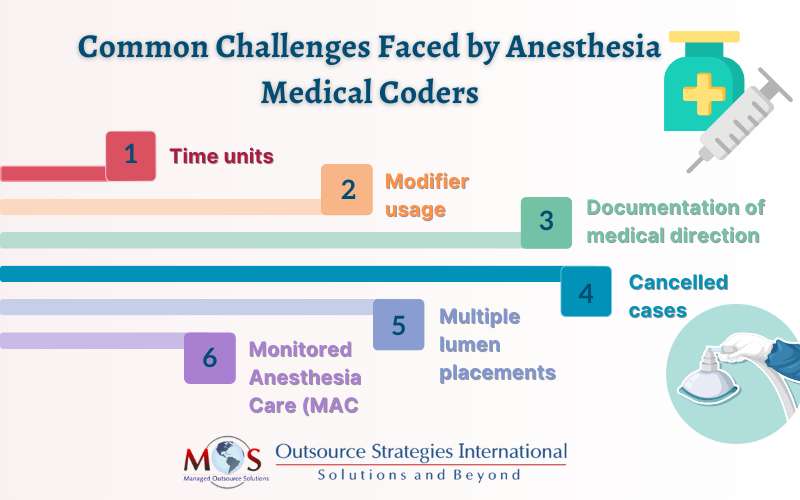
Anesthesia practices need to navigate the complexities present in anesthesia coding successfully for proper reimbursement. These include challenges such as accurately calculating time units, applying appropriate modifiers, and implementing a comprehensive documentation process for an optimized coding process. By ensuring adherence to the latest anesthesia coding guidelines, practices can tackle these challenges with accuracy and compliance. Anesthesia practices can choose to collaborate with a medical billing company that specializes in anesthesia services for streamlining the coding and billing process and ensuring maximum revenue flow.
Challenges in Anesthesia Medical Coding
Focus on patient care while our anesthesia billing and coding experts tackle your anesthesia practice’s billing for maximum cash flow!
Time Units
The most distinctive aspect of anesthesia coding is the calculation of time units as they are essential to reporting anesthesia services for billing purposes. Typically, anesthesia administration is recorded based on time units, in which one unit equals 15 minutes of total anesthesia time. Any errors or discrepancies in reporting the correct anesthesia time can lead to lost revenue, audits, and even penalties for fraud practices. Coders need to confirm that the reported time is not exceeding the average turnover time when there isn’t necessary documentation that explains why the physician spent that much time with the patient. When coding, it is essential to remain very cautious in the following instances:
- Start time: Anesthesia start time is defined when the anesthesiologist begins preparing the patient for the induction of anesthesia services such as pre-operative sedation, placement of monitors, and other activities. However, any activity, such as reviewing the medical history of the patient before surgery is not billable under anesthesia start time as they are part of the preoperative evaluation.
- Stop Time: Anesthesia stop time is when the anesthesia provider is no longer in personal attendance and transfers care to a post-anesthesia care unit under another specialist. The time spent rendering service in the PACU is billable up to a maximum of seven minutes and any additional amount of time should be justified with an explanation in the patient record.
- Relief time: Relief time or split time basically occurs when a physician takes over a case for another physician in the group where two separate start/stop timelines should be reported on the anesthesia record and charge ticket. Wrong documentation of relief time can cause a compliance problem. The coder should verify the document for this case and bill it in the name of the physician who spent most time with the patient, or who started the case.
- Rounding time: Rounding anesthesia time up or down should be done with great care as imprecision in recording the minutes is one of the major issues that lead to compliance problems. Physician groups often round the time to the nearest 5-minute increment or estimate it on the basis of past experience. However, the start/stop time is to be reported to the nearest minute for Medicare.
- Discontinuous Time: Breaks may occur in anesthesia care when the anesthesia practitioner is no longer in personal attendance with the patient, although the surgical procedure is continued. In these cases, practitioners should report only the total anesthesia time for the sum of the continuous block of anesthesia care. They must document the actual start/stop time and check the discontinuous time box whenever needed. Good documentation should include the blocks of time before and after the interruption (for instance, 9:45 anesthesia out time, anesthesiologist leaves the patient, 10:30 anesthesia in time). Documenting in this way makes it easy for the auditor to understand the continuous and discontinuous periods of anesthesia. It is also important to make sure that the total anesthesia time is obtained after adding up the blocks of continuous time.
Modifier Usage
For every anesthesia procedure, the usage of correct modifiers is crucial as it describes various aspects, such as the patient’s physical status, number of providers, and medical direction. Multiple modifiers can be attached to inform payers about the following condition, including:
- Varying medical condition of the patient
- Indicate the amount of anesthesia providers and their roles
- Type of anesthesia service
- Identify the anesthesia given
- Report any unusual circumstances
Anesthesia coders must carefully evaluate the document of each anesthesia service and append appropriate modifiers to anesthesia procedure codes for maximum reimbursement. Failure to do so may result in consequences such as denial of claims or lost revenue.
Documentation of Medical Direction
Physicians must medically direct qualified providers in two, three or four concurrent cases and perform the following seven steps to bill for medical direction and become eligible for reimbursement.
- Perform a pre-anesthetic examination and evaluation
- Set up an anesthesia plan
- Participate personally in most critical and demanding procedures in anesthesia plan such as induction and emergence
- Make sure that a qualified individual performs every procedure in the anesthesia plan that are not performed personally
- Supervise the course of the administration of anesthesia at frequent intervals
- Be physically present and available in case of immediate diagnosis and treatment of emergency cases
- Provide post-anesthesia care as specified
If any of these steps are not performed or a task which is not permitted in medical direction is performed, then it is reported as medical supervision. The guidelines to be followed for qualifying medical supervision are as follows:
- The anesthesiologist is involved in furnishing more than four procedures concurrently
- The anesthesiologist is performing other services while directing the concurrent procedures. There are several exceptions to this requirement:
- Addressing an emergency of short duration in the immediate area
- Administering an epidural or caudal anesthetic to ease labor pain
- Periodic (rather than continuous) monitoring of an obstetrical patient
- Receiving patients entering the operating suite for the next surgery
- Checking or discharging patients in the recovery room
- Handling scheduling matters
Hence, the physician should document all the details of medical direction correctly.
Cancelled Cases
If a case is cancelled before anesthesia induction, the accurate evaluation and management (E/M) code should be reported along with the reason for the cancellation (for example, due to equipment failure). If it is cancelled after induction, report the code along with the appropriate modifier and time. The modifiers that can be used are:
- -53 for discontinued procedure
- -73 for procedures discontinued before providing anesthesia
- -74 for procedures discontinued after anesthesia administration or after the procedure begins
Unless anesthesiologists document the cancelled cases well, enough information may not be available to select the correct E/M codes and modifiers.
It is also of utmost importance to know which insurers accept modifiers and those that do not. If the carriers are not accepting the modifiers, such cases can be billed using the correct anesthesia code with the full base units and total time documented on the record in which the reason for cancellation is documented clearly.
Multiple Lumens Placement
Anesthesiologists are not paid separate payment for placing multiple lumens unless they did a central venous pressure and a Swan-Ganz with two separate lines or two sticks. But, they are required to document the line placements and monitoring. Never bill the time for the placement of post-operative block or invasive lines before administration of the primary anesthetic for the relevant surgery. Such services should be billed as a flat rate fee. Alternatively, the time spent for the placement of post-operative block or invasive lines should not be subtracted after the administration.
Monitored Anesthesia Care (MAC)
While billing for MAC, give more focus to medical necessity. If a patient loses consciousness at any time, it should be considered as general anesthesia, no longer MAC. As local coverage determination varies according to carriers and changes rapidly, documentation is critical to support diagnoses and ensure reimbursement in the case of MAC.
By successfully navigating the above challenges present in anesthesia coding, practices can reduce administrative burdens, meet compliance standards, and maximize reimbursement. Hiring an anesthesiology medical coding company can be a strategic decision for anesthesia practices to ensure accurate anesthesia coding and billing processes that generate maximum financial outcomes.




