Medical billing refers to the preparation of billing claims and their submission to insurance providers. The medical billing process or the billing cycle in a healthcare practice includes all steps of communication from first registering a patient, through recording any care or treatments administered, to receiving reimbursement for the services rendered.


What’s Slowing Your Practice Down? Is Your Medical Billing Process Perfect?
Maintain financial health with transparent RCM services!
Call (800) 670-2809 Today!
Importance of Accurate Medical Billing
Accurate medical billing services play a key role in ensuring the financial health and stability of healthcare providers. It reflects the services rendered and resources used in patient care. Any inaccuracies can lead to legal and financial repercussions.
Precise medical billing:
- Ensures fair compensation for healthcare providers
- Helps maintain regulatory compliance and coding standards
- Contributes to a transparent and efficient healthcare system
- Facilitates timely reimbursement and minimizes financial strain
- Prevents fraud and abuse within the healthcare system
- Provides patients with transparent information about their healthcare costs

Explore the significance of accurate medical billing and its impact on healthcare providers’ financial health in this informative blog post: Importance of Accurate Medical Billing
Some of the common challenges in medical billing include coding errors, complex and ever-changing healthcare regulations, insufficient training and communication among billing staff and the lack of standardized processes that can lead to confusion and administrative complexities. Addressing these challenges necessitates a proactive approach, ongoing staff training, and the implementation of robust technology solutions to streamline billing procedures and enhance overall revenue cycle management in healthcare settings.
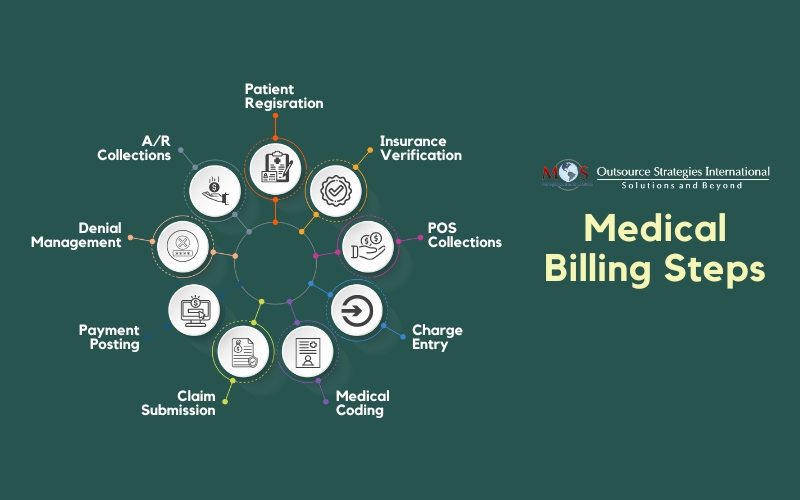
Key Stages in the Medical Billing Process
1. Patient scheduling and registration – Patient scheduling involves the strategic organization of appointments, ensuring that healthcare providers can optimize their resources while minimizing patient wait times. During patient registration, our team will collect and record essential demographic, insurance details, and medical history about a patient when they first seek healthcare services at a healthcare facility. Accurate registration is key for creating a thorough and up-to-date patient record, facilitating effective communication among healthcare professionals, and ensuring accurate billing and reimbursement.
2. Insurance eligibility verification – This step is vital to ensure that the patient’s insurance plan is active and that the services they receive from the provider are covered by the plan. Insurance eligibility verification involves collecting and verifying the patient’s insurance information, including their insurance policy number, group number, and subscriber name with his/her insurance company. By verifying insurance details upfront, healthcare providers can avoid claim denials, reduce billing errors, and streamline the overall medical billing steps.
3. Point of service (POS) collections – POS collections serve as a proactive measure to secure patient payments at the time of service. By collecting co-payments, deductibles, or any outstanding balances during the patient’s visit, healthcare providers can enhance their revenue cycle and reduce the risk of unpaid bills. These collections contribute to financial stability and streamline the billing workflow, minimizing the administrative burden associated with chasing payments after the service is provided.
4. Charge entry – Charge entry involves the systematic recording of healthcare services and corresponding charges for accurate billing and reimbursement. Once the right medical codes are assigned to diagnoses and procedures, the charge entry step ensures that these codes, along with associated fees, are entered into the billing system. It forms the foundation of a claim, providing a comprehensive breakdown of the services provided during a patient’s visit.
5. Medical coding – Medical coding is the translation of complex healthcare services and procedures into universally recognized alphanumeric codes. These codes, typically standardized under systems like ICD-10 (International Classification of Diseases, 10th Edition) and CPT (Current Procedural Terminology), serve as a universal language for healthcare transactions. Trained medical coders review clinical documentation to accurately assign the appropriate codes, ensuring that healthcare providers are reimbursed correctly for the services they provide patients.
6. Claim submission – This process involves the transfer of claims from the healthcare provider to the payer. Typically, claims are initially sent to a clearinghouse, which carefully reviews and reformats the medical claims before forwarding them to the payer. However, in certain instances, healthcare providers may opt to send medical claims directly to a payer. Large-volume payors such as Medicare or Medicaid often receive bills directly from providers, streamlining the reimbursement process and minimizing the time required to receive payment.
7. Payment posting – Payment posting is a crucial step that involves recording and reconciling payments received from insurance companies or patients. Once a claim has been adjudicated, and the insurance provider determines the reimbursement amount, the payment posting phase begins. In this stage, meticulous attention is given to accurately documenting the payment details, including the amounts paid by the insurance company and any patient responsibility, such as co-pays or deductibles. These details are then entered into the billing system, updating the patient’s financial records accordingly.
8. Denial management – When a claim is denied by an insurance company, it signifies that the submitted billing request has been rejected for various reasons, such as coding errors, insufficient documentation, or eligibility issues. Denial management aims to identify the root causes of claim denials, address the underlying issues, and resubmit the corrected claims for reimbursement. This process requires a comprehensive review of denial reasons, effective communication with payers, and timely corrective actions.
9. A/R collections – Accounts Receivable (A/R) collections focus on the systematic pursuit of outstanding payments from insurance companies and patients. After the initial billing and claim submission, healthcare providers must closely monitor the A/R to track unpaid balances. A/R collections involve diligent follow-up on unpaid claims, engaging in communication with insurance providers to resolve discrepancies and address denials.
Benefits of Outsourced Medical Billing Services
Outsourcing medical billing offers diverse benefits to healthcare practices such as professional billing expertise, accurate coding, timely submissions, and accelerated payment cycles. This strategic approach reduces operational costs significantly, allowing healthcare providers to redirect resources toward patient care and practice growth. Additionally, outsourcing ensures compliance with evolving healthcare regulations, minimizing legal risks and fostering financial transparency.
How to Enhance Your Medical Billing Process?
An efficient and accurate billing process in any practice, requires key attention to details. Enhancing your billing function is crucial for improving efficiency, reducing errors, and ensuring timely reimbursement.
Here’s how you can enhance your medical billing process:
Track denials regularly – Regularly tracking denials is vital for the continuous improvement of revenue cycle management. Denials, if left unaddressed, can result in delayed payments and revenue loss for healthcare providers. By systematically monitoring and analyzing denials, you can:
- Identify patterns or trends in the types of denials you are experiencing
- Identify the root cause of claim denials for targeted improvements
Invest in training and education – Provide ongoing training to your billing staff on the latest coding updates, compliance regulations, and industry-best practices. This helps to ensure compliance with healthcare regulations and standards, reducing the risk of audits and penalties.
Regularly update patient information – Keep patient information up-to-date to avoid claim denials due to inaccurate details. Regularly verify insurance information including coverage, addresses, or contact numbers to prevent billing issues. Timely updates also contribute to improved communication between healthcare providers and patients, ensuring that bills and statements reach the correct recipients promptly.
Implement a denial management system – Develop a robust denial management process to identify and address claim denials promptly, reducing the impact on revenue. By understanding these denial trends, providers can proactively implement measures to prevent recurring issues, whether they stem from coding errors, incomplete documentation, or other issues.
Regularly audit billing practices – Conduct regular audits to identify billing errors, compliance issues, and areas for improvement. Address any issues promptly to prevent recurring problems. Audits provide insights into coding accuracy, documentation completeness, and adherence to compliance regulations. Regular audits also contribute to staff training and development, ensuring that billing teams stay informed about the latest coding updates and compliance requirements.
Need support with accurate claims processing? The OSI team can help you optimize your medical claims billing process. We focus on improving your revenue cycle, while you focus on providing quality patient care.

Have questions on the role of documentation in ensuring billing accuracy?
Discuss with our medical billing team! Call (800) 670-2809!