Insurance verification is a crucial element in upholding financial stability and operational efficiency in medical practices. To improve efficiency in insurance verification, it’s essential to confirm patient insurance coverage details and eligibility before delivering medical services. Validating insurance information upfront allows you understand each patient’s insurance coverage and benefits. This helps prevent billing errors and claim denials, and allows you to collect copayments and deductibles in advance. By allowing patients to plan for their care and reducing the chances of surprise bills, verifying insurance coverage also enhances patient satisfaction.
However, the process of checking insurance coverage can be complex and time-consuming, causing inefficiencies and delays. This post outlines efficiency strategies for insurance verification teams to help streamline workflows, improve accuracy, and enhance productivity.

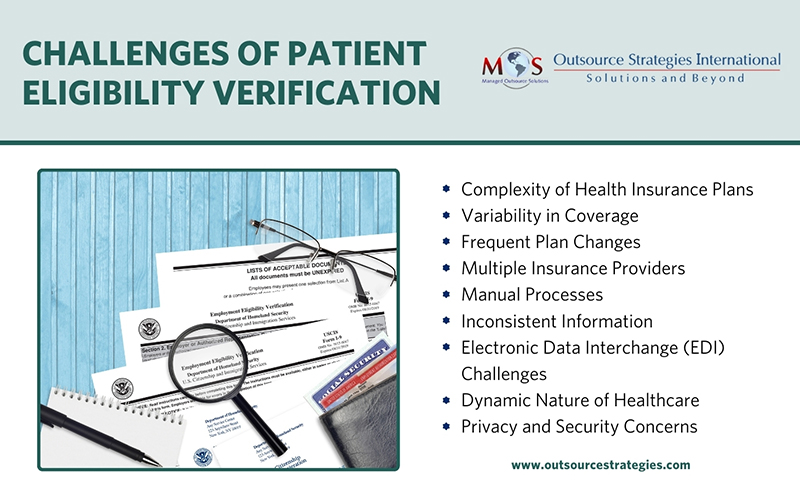
Challenges of Patient Eligibility Verification
Before we discuss how to improve the efficiency of the process, let’s look into the reasons why health insurance can be challenging.
- Complexity of health insurance plans: Health insurance plans come with complex terms, conditions, and coverage details. Each plan may have different coverage levels, exclusions, and requirements, making it difficult to quickly and accurately verify a patient’s coverage.
- Variability in coverage: Even within the same insurance provider, policies may differ in terms of the extent of coverage. Verification requires examining specific details such as deductibles, copayments, coinsurance, and annual limits, which can vary widely among plans.
- Frequent plan changes: Health insurance plans can change frequently, with updates to coverage, network providers, and reimbursement rates. As healthcare providers may not be informed about these changes immediately, it can lead to discrepancies in the information available at the point of verification.
- Multiple insurance providers: Healthcare providers can find it challenging to deal with the diverse payer landscape. Every insurance company has its own set of rules and requirements. Verifying coverage for patients with different insurance providers makes matters even more complex.
- Manual processes: Verifying patient coverage and benefits often involves manual tasks, such as calling up insurance companies or accessing online portals. These manual processes can be time-consuming, prone to errors, and contribute to delays in obtaining accurate information.
- Inconsistent information: If there are discrepancies between the information provided by the patient at the time of registration and the actual coverage details, it can make verification challenging.
- Electronic Data Interchange (EDI) challenges: Electronic data exchange between healthcare providers and insurance companies is not fully standardized. Incompatibility issues and differences in data formats can hamper seamless information exchange. Moreover, the lack of a centralized platform for accessing and verifying insurance information can make the process more fragmented and time-consuming.
- Dynamic nature of healthcare: Healthcare is a dynamic field with constant changes in regulations, billing codes, and technology. Keeping up with these changes and ensuring that verification processes align with the latest standards can be a continuous challenge.
- Privacy and security concerns: The sensitivity of health-related information necessitates secure handling, which can add additional layers of complexity to the verification process. It requires securely storing, transmitting, and disposing of data, along with implementing access controls and authentication measures to deter unauthorized access. Adhering to data protection regulations like HIPAA is essential for upholding trust and avoiding potential legal repercussions.
Addressing these challenges often involves a combination of technological solutions, improved data exchange standards, and ongoing communication between healthcare providers and insurance companies to ensure accurate and timely verification of health insurance coverage.

Ready to optimize your insurance verification process?
Discover best practices for streamlining complex insurance plan verification
Best Practices for Improving Efficiency in Medical Insurance Eligibility Checks
Here are the top features of efficient medical insurance checks:
- Obtaining patient information
During pre-registration, collect demographics, medication lists, other medical history information, insurance information, payments, and consent. With access to patient data, verification specialists have enough time to organize, review, and share information. Add the patient and their insurance information to the EHR or PMS.This early step is essential to streamline the insurance verification process and minimize downstream delays.
- Using a detailed checklist
When the patient arrives for the appointment, use the following checklist to ensure that all the necessary details are collected:
- Name of the patient
- Insurance company and ID
- Phone number and group number
- Claims address
- Policy’s effective date and end date
- Primary and secondary insurance coverage
- Status whether the insurance is currently active
- Whether the insurance covers the services, diagnosis, and procedures to be provided
- Whether your practice participates with the insurance plan
- Limitations and exclusions of the policy
- Referral or pre-authorization requirement
- The patient’s co-pay and deductibles
By utilizing a standardized checklist not only reduces errors, but also supports workflow improvements by reducing the need for follow-up calls or clarifications.
- Verifying patient eligibility with the insurance company
Verification specialists typically contact the payer (insurance company) once they have the patient’s information. This communication is commonly done over the phone, where the insurance information collected from the patient is shared with an authorized insurance representative. The purpose is to confirm the coverage and benefits for the patient, including policy status, deductibles, and co-pays. Phone calls are often considered the more reliable option as they allow for real-time eligibility checking and immediate clarification of any uncertainties.
However, implementing advanced technologies and tools can significantly expedite and improve the efficiency of patient eligibility verification processes. Software tools designed specifically for the purpose cross-reference patient information with insurance databases in real-time and generate electronic reports. Integrating such technology is a critical step in streamlining medical insurance verification processes, especially in high-volume practices.
Overall, both traditional phone calls and advanced technology solutions play a role in these services, and the choice between them depends on the specific needs and preferences of the healthcare organization.
- Establishing clear communication channels
Companies providing patient eligibility checks help providers establish streamlined and standardized communication channels with insurance companies and patients. It involves ensuring secure electronic channels for transmitting insurance information, utilizing standardized forms and documentation, and ensuring timely responses from insurance companies. Clear, consistent communication is one of the most effective workflow improvement strategies for insurance verification teams.

Want to learn more?
Read our post for valuable insights on Front-end optimization in medical insurance verification.
- Centralized data management
Establishing a centralized system for managing patient and insurance information allows for quick access and retrieval. Patient data is updated accurately, ensuring consistency in the verification process. Any discrepancies identified during the eligibility check process are promptly addressed as data inaccuracies in the system can lead to delays lasting days or weeks, or even result in unpaid claims.
- Staff training and development
Continuous improvement in insurance eligibility checks also requires ongoing staff training and skill development. Companies providing these services provide comprehensive training for their staff to ensure that they are well-versed in navigating insurance portals, understanding policy terms, and handling common verification challenges enhances efficiency.
- Robust reporting and analysis mechanisms
Healthcare providers need to implement robust mechanisms to ensure reporting and analysis for continuous improvement in insurance verification. By regularly assessing and analyzing data, medical insurance eligibility checks can be refined and enhanced, leading to increased efficiency and accuracy. Data analytics tools can identify patterns and trends, enabling the implementation of proactive strategies to address issues before they escalate. Detailed reporting can provide insights into potential bottlenecks or areas for improvement. Continuous monitoring and analysis of key performance indicators (KPIs) help in evaluating the effectiveness in eligibility checks, providing valuable information for decision-making.
Efficiency in insurance verification services is crucial to ensure prompt and accurate reimbursement for healthcare services. Providers can streamline their insurance verification processes by partnering with an experienced company. These companies employ professionals with expertise in navigating the complexities of the verification process. As providers focus on delivering quality patient care, leveraging the services of experts can improve workflow efficiency, reduce claim denials, and stabilize cash flow.


Experience precision, efficiency, and peace of mind with our insurance verification services!