Healthcare revenue cycle management (RCM) is the process of managing the financial aspects of healthcare services, from patient registration and appointment scheduling to the final payment collection. By optimizing each stage of the revenue cycle management in medical billing, practices can minimize billing errors, reduce claim denials, accelerate reimbursement cycles, and enhance the overall financial performance. Efficient front-end revenue cycle strategies for patient scheduling, eligibility verification, charge capture and patient collections are crucial for accurate and timely claims submission and revenue generation.
Healthcare Revenue Cycle Management Benefits
- Efficient claim submission
- Reduced denials
- Improved patient satisfaction
- Faster reimbursement cycles
- Enhanced financial performance
- Workforce optimization
- Compliance


Unlock the full potential of our revenue cycle management services for streamlined medical billing!
Speak to our experts at (800) 670-2809
Key Components of Revenue Cycle Management
Here are key elements of RCM in healthcare:
Patient registration: This crucial phase involves capturing accurate and comprehensive patient information, including demographic details, insurance coverage, and contact information. The effectiveness of patient registration directly influences downstream RCM activities, impacting claim submission, reimbursement, and overall financial outcomes. Electronic health records and automated registration systems help healthcare organizations streamline the process, minimize data entry errors, and improve efficiency.
Patient eligibility verification: Insurance verification process involves confirming and validating a patient’s insurance coverage details. Conducting thorough insurance verification lays the foundation for the subsequent stages of the revenue cycle. Accurate verification helps prevent claim denials and delays by identifying potential issues early on, such as lapsed coverage or pre-authorization requirements.
Patient appointment scheduling: Efficiently scheduling and managing patient appointments is critical to optimize resource utilization and reduce no-show rates, contributing to a steady revenue stream. This process involves coordinating and arranging appointments for medical consultations, examinations, or treatments. Modern healthcare systems often use technology such as appointment scheduling software and online platforms to streamline the process, helping patients book appointments conveniently and allowing healthcare providers to manage their schedules more effectively.
Charge capture: Charge capture involves accurately capturing and coding medical procedures, tests, and services performed during a patient encounter. This ensures that all billable services are accounted for in the billing process.
Coding and documentation: Medical coding is translating the details of patient encounters, diagnoses, and treatments into standardized codes, such as ICD-10 (International Classification of Diseases, 10th Edition) and CPT (Current Procedural Terminology). As these codes serve as the language through which healthcare providers communicate with payers, accurate and thorough medical coding is crucial for proper claims submission and reimbursement.
Claim submission: Claims processing in healthcare involves compiling and submitting detailed information about the healthcare services provided to patients to insurance payers for reimbursement. Accurate and timely claim submission is imperative for the financial health of healthcare organizations, as it initiates the process through which providers receive payment for their services. The information submitted includes coded data related to diagnoses, treatments, and procedures performed during patient encounters.
Patient billing and collections: This crucial phase in RCM involves generating clear and comprehensive patient statements detailing the costs associated with medical treatments, consultations, or procedures. It also includes implementing effective strategies to recover unpaid balances, such as setting up payment plans or facilitating discussions about financial assistance options. This helps improve cash flow and reduce bad debt, contributing to efficient RCM.
Accounts receivable (AR) management: This process involves monitoring and managing the receivables, which include unpaid claims, outstanding patient balances, and other accounts awaiting reimbursement. An effective follow-up process is implemented for unpaid claims and overdue patient payments. The primary goal of AR management is to ensure the timely and efficient collection of payments, enhancing cash flow and maintaining financial stability.
Payment posting: Payment posting plays a vital role in maintaining the integrity of the financial records, providing transparency, and facilitating efficient accounting. During this process, financial transactions are accurately documented, matching received payments with corresponding claims and invoices. This step ensures that financial records accurately reflect the revenue generated from healthcare services.
Denial management: A claim denial occurs when the payer has not accepted the request for reimbursement. This occurs due to errors, inaccuracies, or non-compliance with their policies. Effective denial management strategies are crucial to analyze and address claim denials promptly, identify root causes and implement corrective measures to reduce future denials. Using technology and analytics, this process enhances the transparency of billing processes, reduces the time and effort spent on appeals, and ultimately contributes to a more streamlined and effective revenue cycle.
Financial reporting and analytics: Financial reporting in healthcare refers to the systematic analysis and interpretation of financial data to generate insights and inform strategic decision-making. This process involves the compilation, examination, and presentation of financial information, including revenue, expenses, and key performance indicators, in a format that facilitates understanding and decision support.

Want more content like this?
Read our post on Financial Reporting and Analysis for Healthcare Providers
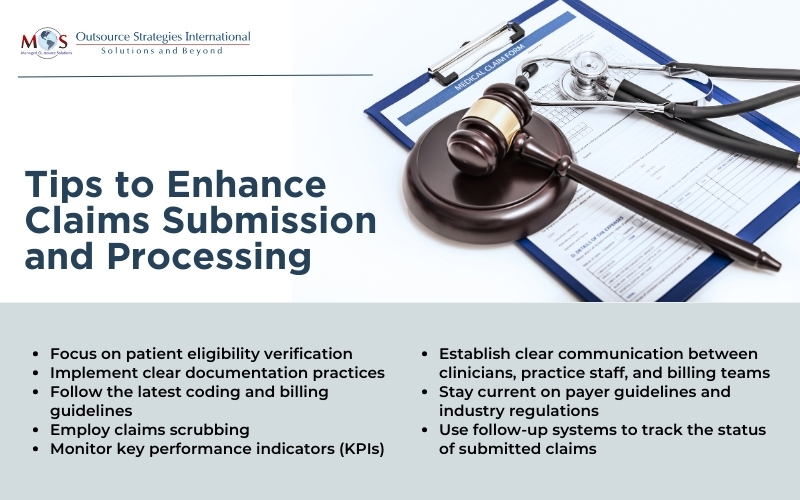
Streamlining Claims Submission and Processing
An efficient and well-organized claims process accelerates the reimbursement cycle, ensuring that healthcare providers receive timely payments for services rendered. Practices are using a blend of coding and revenue cycle management (RCM) services to guarantee the initial precision of claim codes. This strategy allows for the submission of error-free claims with accurate codes and modifiers, thereby improving the entire claims process. The utilization of AR follow-up services plays a crucial role in recognizing persistent issues and patterns, such as submitting claims to the wrong payer address or overlooking payer-specific requirements. Additionally, it assists in identifying consistent denials and addressing other challenges in the process. By streamlining claims submission and processing with proven strategies, providers can maintain consistent cash flow and increase investment in strategies to improve patient care.
Partnering with a professional medical billing company is a practical approach to enhance revenue cycle management. These companies specialize in navigating complex billing processes, streamlining the submission of claims, and ensuring accurate coding and billing practices. By outsourcing these tasks to experts, healthcare professionals can focus more on patient care while experienced professionals manage the intricacies of billing for optimal reimbursement.